Here's a case you don't see every day - and it all starts with a single dose of over-the-counter cold medicine.
Case
A 23-year-old male presented to the hospital complaining of odynophagia which he first noticed prior to his presentation to the ED, and which occurred after ingesting a single over-the-counter cold medication. Prior to taking the gel capsule which contained acetaminophen, dextromethorphan, guaifenesin, and phenylephrine HCl, the patient had a sore throat and no difficulty swallowing. The patient reported difficulty swallowing the gel capsule but an inability to expel it. Afterward, the patient attempted to swallow liquids but was unable to do so. He had no difficulty breathing or speaking. He denied retching, vomiting, drooling, abdominal pain, chest pain, cough, shortness of breath, hemoptysis, recent travel, recent illness, other new medications, new foods, excessive alcohol use, drug use, or smoking. His last meal was at 7 pm the day prior.
His initial vital signs were a temporal temperature of 97.8 F, blood pressure of 128/70 mmHg, heart rate of 97 beats per minute, respiratory rate of 20 breaths per minute, and oxygen saturation of 100% on room air.
The physical examination revealed a well-appearing male who was in no distress and with a patent airway without stridor. His oral mucosa was moist with no pooling of secretions. On examination of the oral cavity, no foreign bodies or obvious oral lacerations were noted, and his dentition was intact with no abnormalities. The patient demonstrated normal phonation and was tolerating secretions without difficulty. No neck masses, asymmetry, bruising, or rashes were identified, and no thyroid enlargement, asymmetry, or nodules were noted. There was no jugular venous distention and no lymphadenopathy. His heart sounds were normal, and lungs were clear to auscultation with no wheezing, rhonchi, or rales. There was no chest wall tenderness or sternal crepitus. The abdomen was nontender and bowel sounds were present. The patient was alert, awake, and oriented and had no neurological deficits. He was given 30 mL of aluminum and magnesium hydroxide-simethicone, 15 mL of 2% lidocaine oral solution swish and spit, followed by 5 mL phenobarbital-hyoscyamine-atropine-scopolamine, all of which did not alleviate his symptoms.
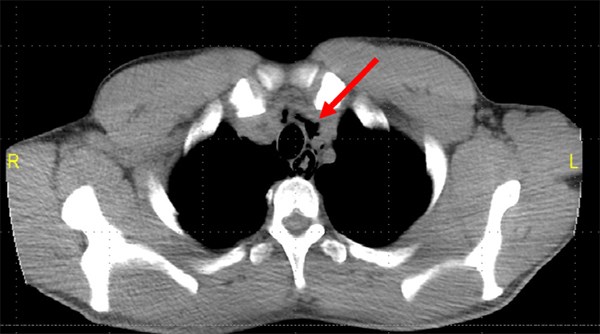
A soft tissue x-ray of the neck revealed no foreign body, but there was questionable linear retropharyngeal extraluminal gas noted. Due to this finding, Computed Tomography (CT) of the neck was performed without contrast and identified a non-obstructing soft tissue density and pneumomediastinum with parapharyngeal gas in the neck. Chest x-ray confirmed a faintly visualized pneumomediastinum, and Gastroenterology was consulted. After evaluating the patient, the gastroenterology team recommended an esophagram to assess for esophageal perforation.
An esophagram with barium contrast confirmed the pneumomediastinum but was unable to identify a site of perforation with no fluoroscopic evidence of contrast extravasation. However, given preceding imaging confirmed a pneumomediastinum as well as air within the wall of the esophagus, suspicion remained high for an esophageal injury. A CT of the chest without contrast was performed and further confirmed the pneumomediastinum extending mostly around the esophagus to the level of the gastroesophageal junction with no new acute changes. Oral contrast from the previous esophagram was identified within the central portion of the distal esophagus which was reported as intraluminal. No contrast extravasation into the mediastinum was identified. Also noted was air within the wall of the proximal stomach as well as a few droplets of apparent extraluminal air posterior to the stomach in the left subdiaphragmatic region. This air was likely secondary to extension from the pneumomediastinum/paraesophageal air. No free contrast was identified in the upper abdomen.
The patient’s EKG revealed a normal sinus rhythm with a heart rate of 75 bpm with no ST changes or QT prolongation. Labs were drawn, including a CBC, BMP, PT/PTT, and the only appreciated pertinent lab finding was a leukocytosis with a WBC of 15.41. Otherwise, all other lab results were within the normal range. The patient was started on intravenous Normal Saline fluids and 3.375 g of IV piperacillin-tazobactam was administered for broad-spectrum antibiotic coverage. The patient was then admitted to the Medical Intensive Care Unit (MICU) for further monitoring, and he was not allowed anything by mouth (NPO).
Figure 1: CT neck without contrast, revealing pneumomediastinum
Figure 2. CT chest without contrast, demonstrating free air around the esophagus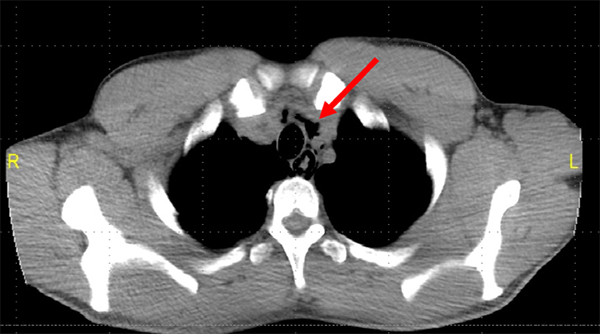
Figure 3. Esophagram revealing pneumomediastinum
Discussion
Esophageal perforation is a full-thickness tear in the esophageal wall.1 The esophagus lacks a serosal layer, thus making it more vulnerable to injury.2 The vast majority of perforations are caused by medical instrumentation.1.2,3 Other common causes include trauma, post emesis injury, esophageal disease, and caustic liquids.2 An ingested substance, whether it be food, foreign body, or medication, rarely causes a perforation. The rarity of which is what makes this case of suspected medication-induced esophageal perforation interesting.
Patients presenting with esophageal perforation can have a variety of signs and symptoms. Patients can present with symptoms including but not limited to chest pain, dyspnea, vomiting, hematemesis, dysphagia, neck pain, odynophagia, hoarseness of voice, and shoulder pain.2 Physical exam findings are generally benign, though it can be possible to note crepitus, local tenderness, or subcutaneous emphysema. The diagnosis is primarily made with the use of imaging. A Chest X-Ray is performed to evaluate for free air and for pleural effusions. An esophagram is performed with contrast to identify an esophageal perforation by evaluating for contrast extravasation. Complications of esophageal perforation include mediastinitis, an intrathoracic abscess, shock, respiratory failure, and pneumomediastinum. Treatment depends on symptom severity, patient presentation, and on the patient’s clinical course. Given the possibility of deterioration and for significant complications, as listed above, patients commonly require ICU admission, NPO status, and observation.
Pneumomediastinum, also known as mediastinal emphysema, is the presence of air in the mediastinum.4,5 It can result from barotrauma, direct trauma, or bowel trauma.6 Patients present most commonly with chest pain, which is usually retrosternal. Other common symptoms include shortness of breath (75%), cough (80%), vomiting, and difficulty swallowing.6,7,8 A common finding on physical exam is Hamman’s crunch, which is a “crunching” sound noted on auscultation over the precordium.6,7,8 The diagnosis of pneumomediastinum can be made through plain films. An anteroposterior (AP) chest x-ray can demonstrate lucent streaks or air tracking along mediastinal structures.8 A chest CT can help to assess the extent of the injury and can aid in the confirmation of the diagnosis. Further testing is usually not necessary.8 Laboratory studies and an EKG are reviewed to evaluate for other possible etiologies. The clinical course commonly follows the spontaneous or assisted reabsorption of the free air and thus treatment most commonly consists of observation and supportive care.
In this case, the patient’s presenting complaint of difficulty swallowing, medically termed odynophagia, lead us to evaluate for an esophageal pathology. An x-ray of the neck was ordered to assess for a possible foreign body, which instead noted retropharyngeal air. The radiograph finding and absence of a foreign body prompted further imaging with a CT of the neck for a better evaluation of the upper airway and of the upper gastrointestinal tract. Although the CT scan identified a soft tissue density as the possible inciting cause of the patient’s symptoms and imaging results, the incidental pneumomediastinum warranted further evaluation with an esophagram. Neither CT imaging nor the esophagram identified a perforation with no demonstrated extravasation of contrast. However, the esophagram noted free air in the esophageal wall thereby further supporting that the patient’s pneumomediastinum was induced by an esophageal injury.
The active ingredients in this particular brand of gelcap-acetaminophen, dextromethorphan, guaifenesin, and phenylephrine HCl-are not known to be caustic. Most cases of medication-induced esophageal injury heal without intervention and within a few days.1 In this patient’s case, the esophagram noted air in the esophageal wall, but the repeated CT chest, performed afterward, only noted air within the stomach wall and posterior to the stomach. The combination of these findings suggests that the perforation had initially been large enough to allow free air into the mediastinum, but small enough to have healed within hours and thereby precluding the identification of perforation on further imaging.
Pneumomediastinum, in the context of microperforation, presents similarly to spontaneous pneumomediastinum and will likely resolve on its own. An accurate diagnosis of pneumomediastinum was made through the combination of multiple imaging studies. As explained above, imaging confirmed the presence of free air, but likely due to a healed perforation, could not identify a perforation. The source appears to have been through an esophageal microperforation that healed within hours as demonstrated by a lack of fluoroscopic contrast extravasation on esophagram imaging. Esophagram and CT chest found no extravasation of contrast to neither locate nor confirm perforation.
Case Conclusion
Once the patient was able to tolerate clear liquids, 2 days after MICU admission, he was transferred to the medicine floor. The following day, while on the general medical floor, the patient tolerated a soft diet and was medically cleared by the gastroenterology team for discharge home. In total, the patient spent three nights in the hospital.
Summary
The patient in this report had a good outcome. The patient tolerated oral fluids within 48 hours and was discharged within 72 hours without direct medical or surgical intervention. As in most other cases of medication-induced esophageal perforation, this patient’s injury healed on its own within a few hours to days.4,10 Long term follow up will likely not be necessary as previous studies have noted that the occurrence of reinjury from a non-caustic offending agent, particularly a substance the patient had previously ingested, is low.4,9,10
To our knowledge, there does not appear to be any reported cases of esophageal perforation due to the ingestion of a non-caustic, over-the-counter medication causing pneumomediastinum. Previous reports have commonly attributed the diagnosis of medication-induced esophageal injury to caustic fluids, certain antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, bisphosphonates, potassium chloride, and iron.9,11
While finding the root cause of pneumomediastinum can be important regarding further management and interventions, the treatment goal regarding the diagnosis of pneumomediastinum should be to ensure patient stability through observation and to intervene with resuscitative measures if indicated throughout the patient’s clinical course.
TAKE-HOME POINTS
• Esophageal microperforations can heal within a matter of hours, masking the root cause of pneumomediastinum.
• There appear to be no previously reported cases of a non-caustic, OTC medication leading to pneumomediastinum.
References
- Michel L, Grillo HC, Malt RA. Esophageal perforation. Ann Thorac Surg. 1982;33(2):203-210.
- Mueller DK, Govil Y, Kowalski T, Milliken JC. Esophageal Rupture: Background, Anatomy, Pathophysiology. Available at: https://emedicine.medscape.com/article/425410-overview
- 3. Søreide JA, Viste A. Esophageal perforation: diagnostic work-up and clinical decision-making in the first 24 hours. Scand J Trauma Resusc Emerg Med. 2011;19:66.
- Takada K, Matsumoto S, Hiramatsu T, et al. Spontaneous pneumomediastinum: an algorithm for diagnosis and management. Ther Adv Respir Dis. 2009;3(6):301-307.
- Al-Mufarrej F, Badar J, Gharagozloo F, Tempesta B, Strother E, Margolis M. Spontaneous pneumomediastinum: Diagnostic and therapeutic interventions. J Cardiothorac Surg. 2008;3:59.
- Kouritas VK, Papagiannopoulos K, Lazaridis G, et al. Pneumomediastinum. J Thorac Dis. 2015;7(Suppl 1):S44-S49.
- Macia I, Moya J, Ramos R, et al. Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg. 2007; 31(6):1110-1114.
- Caceres M, Ali SZ, Braud R, Weiman D, Garrett Jr HE. Spontaneous pneumomediastinum: a comparative study and review of the literature. Ann Thorac Surg 2008;86:962-966.
- Castell, DO. Medication-induced esophagitis. Up To Date Available at: https://www.uptodate.com/contents/medication-induced-esophagitis.
- Banki F, Estrera AL, Harrison RG, et al. Pneumomediastinum: Etiology and a guide to diagnosis and treatment. Am J Surg. 2013;206(6):1001–1006.
- Zografos GN, Georgiadou D, Thomas D, Kaltsas G, Digalakis M. Drug-induced esophagitis. Dis Esophagus. 2009;22(8):633-637.