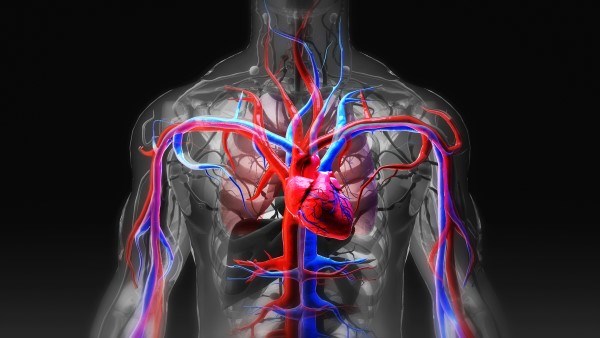
Purpose of MCS
A mechanical circulatory support (MCS) device is a surgical option for patients who have had unsuccessful experiences with optimal medical therapies for advanced heart failure. These therapies ideally bridge a patient from acute onset to long-term cardiac transplantation. But for patients ineligible for transplants, MCSs are a lifeline for cardiac support and allow improved quality and functional status for survival.1
The Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) reports more than 15,000 patients received durable MCSs between June 2006 and December 2014, with a 1-year and 2-year survival rate of 80% and 70%, respectively.2
In the acute setting of cardiogenic shock or cardiorespiratory failure secondary to advanced heart failure, short-term and intermediate-term MCS may be used to escalate therapy when optical medical management has failed. These modalities are typically in place for 30 or fewer days. They are widely used during electrophysiology and interventional cardiology procedures.3
Temporary MCSs are indicated in patients when recovery is expected (bridge-to-recovery) or more time is needed to decide definitive treatment when an outcome is unknown (bridge-to-decision).4
Contraindications generally include patients who would not benefit from a bridging therapy due to severe irreversible end-organ damage, disseminated malignancies, peripheral vascular disease, or any contraindication for anticoagulation.
Each individual device has specific contraindications and specific functions.5 Three of the most popular modalities include intra-aortic balloon pump (IABP), Impella, and extracorporeal membrane oxygenation (ECMO).
Intra-Aortic Balloon Pump
IABP counterpulsation is the most commonly used temporary MCS device in patients with cardiogenic shock and myocardial ischemia.6 About 15-30% of all IABP is used in patients after cardiac surgery requiring cardiopulmonary bypass.
The balloon is inserted into the proximal descending aorta, then rapidly inflates during diastole and deflates during systole. Inflation of the balloon augments diastole by increasing preload, thus increasing perfusion to the coronary arteries and perfusion. Rapid deflation of the balloon causes reduced left ventricle (LV) afterload and LV end-diastolic pressure, therefore decreasing myocardial oxygen consumption and work by decreasing the isovolumic phase of ventricular systole.7 The resulting increase of the myocardial perfusion, despite not fully increasing systemic blood flow, increases cardiac output (CO) by 20%.6 The IABC is traditionally placed via the femoral artery; however, it can be placed in the brachial or subclavian arteries as well. In even more rare cases of severe peripheral vascular disease or repaired aortic dissection, the left axillary artery or aortic arch can be accessed.8
Impella
The Impella pump works by fully offloading the LV and improving blood flow to the myocardium while reducing oxygen demand on the heart. Commonly, it is used in cases to treat postcardiotomy shock. This improves coronary flow and decreases microvascular resistance.9 This unloading of the LV is critical, and in pig studies has been found to decrease the baseline infarct size by 5 times in LAD occlusions.9 If necessary, a right ventricular Impella may be placed.
The Impella requires a constant infusion of heparin directly into the pump at about 25% of the ECMO requirement.9
Ideally it is placed via right femoral artery access, as it is the fastest site to obtain. Axillary arterial insertion requires surgical intervention, but is a more permanent solution on patients waiting for transplantation or requiring longer stays.10
ECMO
Venous-arterial (VA) extracorporeal membrane oxygenation (ECMO) is the fastest way to improve circulation in a patient with acute cardiogenic shock and prevent end-organ failure. VA ECMO provides support to the heart and lungs; however, it does not unload the work of the left ventricle. ECMO provides a temporary solution to a more definitive intervention by extracting venous blood from a large vein, passing through an oxygenation circuit, and returning through a large artery.11
Femoral and internal jugular arteries and veins are the preferred location.
VA ECMO indications for cardiogenic shock include fulminant myocarditis, acute myocardial infarction, post-cardiotomy, and post-heart transplantation. Venous-venous (VV) ECMO, however, only provides lung support and involves 2 large vein cannulations.12 It serves as a therapeutic notion in patients with severe respiratory failure and supports systemic circulation. Although this system provides oxygenation to patients in cardiac or respiratory failure, it is highly dependent on patients’ hemoglobin and blood flow status. Therefore, hemoglobin must be maintained above 12.13
Treatment Considerations
- All patients receiving these procedures must also receive full anticoagulation with heparin. Therefore, there must be NO contraindications for anticoagulation.
- The practitioner must be mindful of where intravenous lines are being placed prior to initiation of MCS, to not cause hematomas or excessive damage to large vessels required for cannulation or placement of device.
- Multiple devices may be inserted to be used simultaneously by an electrocardiologist.
- Most hospitals do not have these modalities and require the patient to be transferred to a tertiary care center. Consultation calls should be made to specialists early on in the course of patient stay, even during cardiac arrest in specific cases such as ventricular storm.
References
- Cook JL, Colvin M, Francis GS, et al. Recommendations for the use of mechanical circulatory support: Ambulatory and community patient care: A scientific statement from the American Heart Association. Circulation. 2017;135(25). doi:10.1161/cir.0000000000000507
- Kirklin JK, Naftel DC, Pagani FD, et al. Seventh INTERMACS annual report: 15,000 patients and counting. The Journal of Heart and Lung Transplantation. 2015;34(12):1495-1504. doi:10.1016/j.healun.2015.10.003
- Abnousi F, Yong CM, Fearon W, Banerjee D. The evolution of temporary percutaneous mechanical circulatory support devices: A review of the options and evidence in cardiogenic shock. Current Cardiology Reports. 2015;17(6). doi:10.1007/s11886-015-0594-8
- Department of Internal Medicine Division of Cardiology. Ventricular assist device therapy for heart failure-past,... : International Anesthesiology Clinics. LWW. https://journals.lww.com/anesthesiaclinics/Citation/2012/05030/Ventricular_Assist_Device_Therapy_for_Heart.8.aspx. Accessed March 15, 2023.
- NK; MJACHMSK. Temporary mechanical circulatory support devices: Updates from recent studies. Current opinion in cardiology. https://pubmed.ncbi.nlm.nih.gov/33990478/. Accessed March 15, 2023.
- González LS, Chaney MA. Intraaortic balloon pump counterpulsation, part I: History, technical aspects, physiologic effects, contraindications, medical applications/outcomes. Anesthesia & Analgesia. 2020;131(3):776-791. doi:10.1213/ane.0000000000004954
- González LS, Chaney MA. Balloon pump counterpulsation part II: Perioperative Hemodynamic Support and new directions. Anesthesia & Analgesia. 2020;131(3):792-807. doi:10.1213/ane.0000000000004999
- Wu IY, Wyrobek JA, Naka Y, Dickstein ML, Glance LG. Perioperative management of patients receiving short-term mechanical circulatory support with the transvalvular heart pump. Anesthesiology. 2022;136(5):829-842. doi:10.1097/aln.0000000000004124
- Gässler H, Kurka L, Rauch S, Seewald S, Kulla M, Fischer M. Mechanical chest compression devices under special circumstances. Resuscitation. 2022;179:183-188. doi:10.1016/j.resuscitation.2022.06.014
- Bero M, Sochor M, Wong S, Brady W. Changing the management of refractory ventricular fibrillation: The consideration of earlier utilization of dual sequential defibrillation. The American Journal of Emergency Medicine. 2020;38(3):545-548. doi:10.1016/j.ajem.2019.05.048
- Pionkowski RS, Thompson BM, Gruchow HW, Aprahamian C, Darin JC. Resuscitation time in ventricular fibrillation — a prognostic indicator. Annals of Emergency Medicine. 1983;12(12):733-738. doi:10.1016/s0196-0644(83)80245-5
- Ewy GA. Cardiocerebral resuscitation, defibrillation, and cardioversion. Cardiac Intensive Care. 2010:652-671. doi:10.1016/b978-1-4160-3773-6.10052-7
- Lorusso R, Whitman G, Milojevic M, et al. 2020 eacts/Elso/STS/AATS expert consensus on post-cardiotomy extracorporeal life support in adult patients. ASAIO Journal. 2020;67(1). doi:10.1097/mat.0000000000001301