A 50-year-old woman with a history of primary pulmonary hypertension with right ventricular dysfunction presents with one week of worsening abdominal pain. She is lethargic, febrile to 102.5 F, breathing at a rate of 40, and saturating 85% on room air. Her MAP ranges from 60 to 70 mmHg. You pause for a moment as you contemplate fluid management and the risks associated with intubating this likely septic patient with known right ventricular dysfunction.
Introduction
Acute right ventricular (RV) failure, while far less common than left ventricular (LV) failure, adds unique complexity to the management of the critically ill patient. Hypoxia and hypotension can be seen in both decompensated LV and RV failure because of a number of underlying insults. However, the underlying pathophysiology and management considerations differ dramatically.
Physiology Primer
The RV is part of a low-pressure system that is built for compliance and does not handle increased afterload, or pulmonary hypertension, very well. While the RV can adapt through hypertrophy in the same way the LV adapts to systemic hypertension, contractility falls due to dilation in situations of acutely increased afterload (as in acute massive pulmonary embolism), or at the extremes of chronically increased afterload (as in patients with severe COPD, primary pulmonary hypertension, or severe left heart failure).1-4
A severely dilated RV will push the interventricular septum into space otherwise occupied by the LV. This is the concept of “ventricular interdependence.” In decompensated RV failure with volume overload, the interventricular septum shifts into the LV during end-diastole, resulting in decreased LV preload.5 As systemic blood pressure falls and becomes closer to the right ventricular pressure, the pressure gradient over which the RV is perfused is smaller, and the RV is susceptible to ischemia. Once ischemic, the RV contractility falls further, and the sequence self-perpetuates.6-8
Diagnosis
While definitive diagnosis of pulmonary hypertension requires right heart catheterization and invasive measurement of intracardiac and pulmonary artery pressures, bedside echocardiography provides a modality to quickly identify RV dysfunction in the undifferentiated critically ill patient.
The apical four-chamber view, if attainable, is best for comparing chamber size. An RV:LV chamber size ratio >1 or an RV end-diastolic diameter >30 mm (at mid-level) indicate the RV is dilated and THAT right sided pressures may be elevated (Figure 1).9 Likewise, loss of inferior vena cava (IVC) inspiratory collapse indicates increased RA filling pressures seen in decompensated RV dysfunction. In the parasternal short axis view, flattening of the interventricular septum causes the LV to take on a characteristic “D” shape, illustrating the presence of ventricular interdependence (Figure 2).
Fluid Management
In decompensated RV failure, a cautious approach to fluid management is paramount, and it is problematic to rely on one marker of volume status. For example, the IVC may be plethoric in both hypo- and hyper-volemia as a result of increased preload and a non-compliant right heart.
In clinical scenarios suggestive of volume overload (eg, missed dialysis), forward flow can be improved by offloading the RV. Diuretics and even renal replacement therapy can be important.10
In circumstances of hypovolemia, cardiac output may benefit from the cautious administration of IV fluids. Knowledge about the clinical scenario (eg, diarrhea) is critical and may offer the best insight into the patient's volume status. If the volume loss is suspected, the use of small fluid challenges and close monitoring for response is a reasonable approach. Alternatively, performance of a passive leg raise with an associated increase in cardiac output measured via dedicated monitor or bedside echocardiogram may identify a patient as fluid responsive and can guide volume resuscitation. (For more, see “Assessment of Fluid Responsiveness in the ED,” at emresident.org/ahead-curve-assessment-fluid-responsiveness-ed.)
Vasopressors and Inotropes
The RV is perfused in systole and diastole over the pressure gradient between the systemic blood pressure (SBP) and the RV chamber pressure (RVP). In an effort to prevent RV ischemia, systemic hypotension must be avoided so that this pressure gradient is maintained. Unfortunately, many of the commonly used vasoactive agents used to abate systemic hypotension non-selectively cause vasoconstriction, thereby increasing the pulmonary vascular resistance and RV pressure.
Phenylephrine is a pure alpha-1 agonist which acts on the pulmonary vasculature and increases RV afterload; it is best avoided in RV failure. Norepinephrine, in contrast, has been demonstrated to increase the pulmonary vascular resistance less than phenylephrine while augmenting inotropy through beta-1 agonism.11 Vasopressin is an attractive agent for use in RV failure as it is a potent systemic vasoconstrictor but has little effect on the pulmonary vasculature.12 The inodilators — dobutamine and milrinone — augment RV contractility and can have a role when other agents have failed. However, both agents can drop systemic vascular resistance and generally necessitate concurrent use of another vasopressor. Epinephrine offers beta-1,2, and alpha-1 agonism, balancing inotropy with vasoconstriction and providing a standalone agent that increases cardiac output without concern for vasodilation and hypotension. Of note, dobutamine, milrinone, and epinephrine are all potentially arrhythmogenic, which presents unique concerns in patients with RV failure whose cardiac output is dependent on being in sinus rhythm.13,14
Airway Management
Respiratory failure in right ventricular failure is particularly difficult to manage; and intubation should be avoided if possible. This group of patients is prone to peri-intubation hemodynamic collapse due to an increase in RV afterload with positive pressure ventilation and the decrease in systemic vascular resistance on induction.15,16 An ideal strategy for airway management involves optimizing hemodynamics prior to intubation, choosing an appropriately dosed induction agent with a good hemodynamic profile, and using a low-tidal-volume strategy with the avoidance of hypercapnia, hypoxemia, and excessive PEEP. Anticipate post-intubation hypotension. Non-invasive ventilation is an attractive option as it can offer information about how the patient responds to positive pressure and can be easily discontinued.
Adjunctive Therapies
In critically patients with decompensated RV failure who have not responded to other therapies, inhaled nitric oxide should be considered. Nitric oxide selectively dilates the pulmonary vasculature – both decreasing pulmonary vascular resistance and improving ventilation perfusion matching by increasing perfusion to well ventilated parts of the lung.17 Inhaled prostacyclins such as epoprostanol or iliprost similarly dilate the pulmonary vasculature, but, unlike nitric oxide, can have systemic effects and should not be initiated without involvement of specialty services.10 Patients with primary pulmonary hypertension maintained on pulmonary vasodilator infusions in the outpatient setting must be continued on these medications, as sudden withdrawal can precipitate rebound pulmonary hypertension and hemodynamic collapse.18 Extracorporeal membrane oxygenation (ECMO) has a role as salvage therapy in decompensated RV failure, and transfer to a center with ECMO capabilities should be considered early.19,20
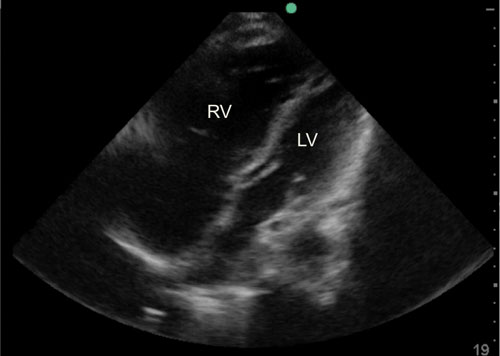 Figure 1. Apical Four Chamber View
Figure 1. Apical Four Chamber ViewRight greater than left ventricular chamber size.
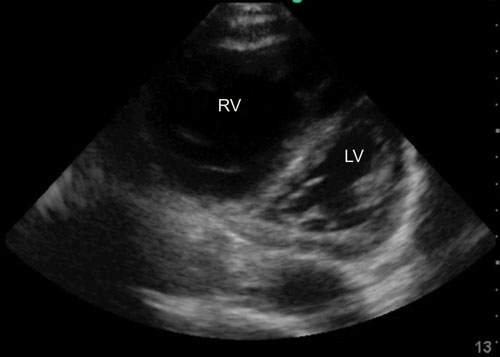 Figure 2. “D” Shaped Septum
Figure 2. “D” Shaped SeptumSeen in diastole indicating RV volume overload and ventricular interdependence.
Case Conclusion
The patient had known right ventricular dysfunction and acutely decompensated due to cholecystitis. She was initially managed with noninvasive ventilation but ultimately required intubation for refractory hypoxia. She had been maintained on subcutaneous treprostinil in the outpatient setting. This was promptly reinitiated as an intravenous infusion. As her systemic blood pressure continued to fall, she was placed on milrinone and epinephrine, as well as inhaled nitric oxide. In the ICU, her condition continued to decline, and transfer to a center with ECMO capabilities was coordinated.
Right ventricular dysfunction adds layers of complexity in the management of the critically ill patient. These patients are susceptible to decompensation in situations of fluid overload, shock states, and other swings in cardiac dynamics. A cautious fluid resuscitation strategy—with care not to iatrogenically overload the RV—is necessary. Systemic hypotension can precipitate RV ischemia and should be avoided with a tailored approach to vasopressor selection and other adjunctive therapies. Intubation comes with a high risk of mortality given the complicated hemodynamic implications of positive pressure ventilation, and should be avoided if possible.
References
- Simonneau G, Robbins IM, Beghetti M, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2009;54(1s1):S43-S54.
- Greyson CR. Pathophysiology of right ventricular failure. Crit Care Med. 2008;36(1 Suppl):S57-65. doi: 10.1097/01.CCM.0000296265.52518.70 [doi].
- Greyson CR. Right heart failure in the intensive care unit. Curr Opin Crit Care. 2012;18(5):424-431. doi: 10.1097/MCC.0b013e3283577070 [doi].
- Gan C, Lankhaar JW, Marcus JT, et al. Impaired left ventricular filling due to right-to-left ventricular interaction in patients with pulmonary arterial hypertension. Am J Physiol Heart Circ Physiol. 2006;290(4):H1528-33. doi: 01031.2005 [pii].
- Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the american society of echocardiography: Endorsed by the european association of echocardiography, a registered branch of the european society of cardiology, and the canadian society of echocardiography. Journal of the American Society of Echocardiography. 2010;23(7):685-713.
- Wilcox SR, Kabrhel C, Channick RN. Pulmonary hypertension and right ventricular failure in emergency medicine. Ann Emerg Med. 2015;66(6):619-628. doi: 10.1016/j.annemergmed.2015.07.525 [doi].
- van Wolferen SA, Marcus JT, Westerhof N, et al. Right coronary artery flow impairment in patients with pulmonary hypertension. Eur Heart J. 2008;29(1):120-127. doi: ehm567 [pii].
- Goldstein JA. Pathophysiology and management of right heart ischemia. J Am Coll Cardiol. 2002;40(5):841-853.
- Matthews JC, McLaughlin V. Acute right ventricular failure in the setting of acute pulmonary embolism or chronic pulmonary hypertension: A detailed review of the pathophysiology, diagnosis, and management. Current cardiology reviews. 2008;4(1):49-59.
- Lahm T, McCaslin CA, Wozniak TC, et al. Medical and surgical treatment of acute right ventricular failure. J Am Coll Cardiol. 2010;56(18):1435-1446.
- Kwak Y, Lee C, Park Y, Hong Y. The effect of phenylephrine and norepinephrine in patients with chronic pulmonary hypertension. Anaesthesia. 2002;57(1):9-14.
- Currigan DA, Hughes RJ, Wright CE, Angus JA, Soeding PF. Vasoconstrictor responses to vasopressor agents in human pulmonary and radial ArteriesAn in vitro study. The Journal of the American Society of Anesthesiologists. 2014;121(5):930-936.
- Anderson JL, Askins JC, Gilbert EM, Menlove RL, Lutz JR. Occurrence of ventricular arrhythmias in patients receiving acute and chronic infusions of milrinone. Am Heart J. 1986;111(3):466-474.
- Kerbaul F, Rondelet B, Motte S, et al. Effects of norepinephrine and dobutamine on pressure load-induced right ventricular failure. Crit Care Med. 2004;32(4):1035-1040.
- Myles PS, Hall JL, Berry CB, Esmore DS. Primary pulmonary hypertension: Prolonged cardiac arrest and successful resuscitation following induction of anesthesia for heart-lung transplantation. J Cardiothorac Vasc Anesth. 1994;8(6):678-681.
- Hoeper MM, Granton J. Intensive care unit management of patients with severe pulmonary hypertension and right heart failure. American journal of respiratory and critical care medicine. 2011;184(10):1114-1124.
- Ichinose F, Roberts JD,Jr, Zapol WM. Inhaled nitric oxide: A selective pulmonary vasodilator: Current uses and therapeutic potential. Circulation. 2004;109(25):3106-3111. doi: 10.1161/01.CIR.0000134595.80170.62 [doi].
- Minai OA, Yared J, Kaw R, Subramaniam K, Hill NS. Perioperative risk and management in patients with pulmonary hypertension. Chest Journal. 2013;144(1):329-340.
- Belohlavek J, Rohn V, Jansa P, et al. Veno-arterial ECMO in severe acute right ventricular failure with pulmonary obstructive hemodynamic pattern. J Invasive Cardiol. 2010;22(8):365.
- Machuca TN, de Perrot M. Mechanical support for the failing right ventricle in patients with precapillary pulmonary hypertension. Circulation. 2015;132(6):526-536. doi: 10.1161/CIRCULATIONAHA.114.012593 [doi].