Lyme disease is one of the most common vector-borne diseases in the United States, affecting over 300,000 people annually between June and December and most prominent in the northeastern, mid-Atlantic, and north-central regions.1
The culprit, Borrelia Burgdorferi, is a spirochete transmitted through deer tick (Ixodes Scapularis) in the Eastern U.S. and the Western blacklegged tick (Ixodes Pacificus) in the West, that gets transmitted to the human host when the tick is attached to the human host for over 36 hours.1
Lyme disease affects every organ system and is described in three progressive stages of disease: early localized, early disseminated, and late disseminated or chronic. Stereotypical manifestations include the cutaneous “bull’s eye rash” (figure 1), unilateral Bell’s Palsy, and Lyme carditis which often causes an AV node conduction abnormality.1,2,3,8 This case report describes a less common cardiac manifestation of Lyme disease: pericarditis with pericardial effusion.
CASE
A 61-year-old female was sent to the ED after an incidental finding of pericardial effusion on outpatient echocardiogram. Her medical history was significant for well-controlled type 2 diabetes, hypertension, and hyperlipidemia. Upon presentation to the ED, the patient endorsed two weeks of intermittent palpitations, worsening dyspnea that was exacerbated by laying down, and weight gain. She denied chest pain, cough, recent fevers or illnesses, any surgeries or long periods of immobilization. Recent travel history was only significant for spending summers at her cabin in Pennsylvania. She denied any family history of cardiovascular disease as well as tobacco, alcohol, or recreational drug use. On the previous week the patient visited her primary care physician (PCP) with these concerns. At that time, atrial flutter was identified on electrocardiogram (ECG). She was started on a beta blocker, an anticoagulant, and referred for the echocardiogram.
Upon further questioning, patient reported she was in her usual state of health until last summer (4 months prior to presentation) when she had developed a single erythematous lesion on the left upper extremity, which eventually spread over her entire body. A skin biopsy was significant for urticaria and she completed a treatment of steroids. She subsequently developed fatigue, then mild positional dyspnea, and 2 months later she developed a unilateral right 6th and 7th nerve palsy. Extensive workup was non-contributory until a spinal tap demonstrated elevated cerebrospinal fluid protein and lymphocytes, when led her PCP to suspect Lyme disease.
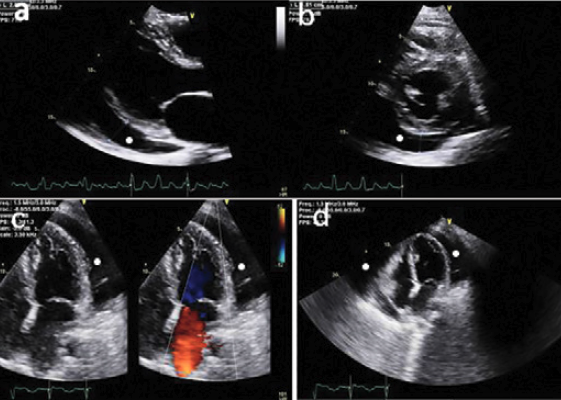
In the ED, her heart rate was 121 bpm, BP 155/65 mmHg, RR 20 breaths/min, and oxygen saturation 100% on room air. Her physical exam was significant for a comfortable appearing woman with an elevated BMI, tachycardia, and moderate bilateral lower extremity pitting edema. Blood work was significant for a WBC 10.9, Hgb 10.5, CRP 33.5, ESR 45. ECG showed atrial flutter with variable block (figure 2), and a bedside echo showed a moderate pericardial effusion without hemodynamic compromise, which was confirmed by formal echocardiography (figure 3). The patient was admitted to cardiology for pericardiocentesis and further work-up.
Figure 2. ECG at presentation demonstrates atrial fibrillation

Figure 3. Pericardial effusion. Transthoracic echocardiogram demonstrates a large pericardial effusion (+) a: Parasternal long axis view demonstrates typical interposition of the pericardial effusion (+) between the heart and the descending thoracic aorta. b: Parasternal short axis at the level of the papillary muscles. c: In the apical 4-chamber view, note that the pericardial effusion surrounds the cardiac apex. d: Subcostal view.
Pericardiocentesis was performed by interventional cardiology and yielded 500 cc of blood so her anticoagulant was discontinued. There was no cytologic evidence of malignancy, viral, bacterial or fungal growth in the pericardial fluid, but have findings consistent with an exudative process with LDH 234 (fluid/serum LDH > 0.6) and fluid protein 76.2 (fluid/serum protein >0.5). Meningitis and respiratory panels, tuberculosis, syphilis, SARS Cov2, and West Nile virus tests were negative. Her Lyme ELISA test resulted 11 days post-admission and was unequivocally positive.
Given her history and presentation, disseminated Lyme disease was thought to have been the cause of her pericarditis complicated by pericardial effusion, and she was presumptively treated for Lyme with 4 weeks of intravenous ceftriaxone. The acute pericarditis was managed with intra-pericardial steroids, ibuprofen, and colchicine. Diuresis was initiated, leading to a 7.7 kg weight loss during her hospitalization and another 10 kg in the subsequent 2 weeks. Her hospitalization was complicated by refractory atrial flutter and decreased cardiac function evidenced by a left ventricular ejection fraction (LVEF) of 30% (from 65% on admission) with global dysfunction. She was discharged on digoxin on hospital day 7 and felt better for a month at which time her symptoms started to return. An echocardiogram at that time revealed interval improvement of cardiac function (LVEF 48%) but a moderate pericardial effusion re-accumulation, managed conservatively with high dose prednisone.
DISCUSSION
Lyme disease is often classified into 3 stages:
First - Early Localized Disease: within days of exposure patients present in the spring or summer with flu-like illness, fever, and a typical rash (erythematous patch with a central scab and blurred margins) (figure 1). The erythema migrans "bull's eye rash" appears within 48 hours and is most apparent 7-14 days after tick is detached.1
Second - Early Disseminated Disease: neurologic manifestations such as Bell’s palsy (unilateral or bilateral) or aseptic meningitis may develop. Cardiac manifestations occur in 1-10 % of cases.1,2,8
Third - Late Disseminated or Chronic: encephalopathy, radiculopathy, severe fatigue, psychologic disturbances, mono-arthralgias (often the knee).1
Evidently, we met this patient on the second stage. “Lyme carditis” most frequently manifests as conduction abnormalities (eg, AV nodal blocks) due to direct toxic and immune-mediated mechanisms. Less commonly, Lyme carditis has been implicated in coronary aneurysms, congestive heart failure, valve disease, ischemic events, endocarditis, myocarditis, and rarely pericarditis (2-5% of Lyme carditis cases in the U.S. and 23% in Europe4,5).
The pericardium consists of thin visceral and parietal layers between which a potential space usually holds 15–35 cc of fluid, but when the pericardium becomes acutely inflamed, a pericardial effusion can ensue and hold up to liters of fluid. Infectious organisms are often the precursor to pericarditis in world, but in north America up to 90% of cases are idiopathic.7 The most common symptoms of pericarditis with effusion are dyspnea, pleuritic chest pain that is relieved by leaning forward and exacerbated by lying down and swallowing, nausea, abdominal pain, and malaise.2,7
Pericardial tamponade is a dangerous complication of the rapid development of a pericardial effusion leading to increased pressure in the pericardial space, decreased ventricular filling and cardiac output leading to hemodynamic collapse. Signs of tamponade can be remembered by the "Beck's triad": hypotension, muffled heart sounds and jugular venous distention.7
The essential workup for pericarditis in the ED includes a physical exam, chest x-ray or bedside ultrasound, ECG, and basic labs. An auscultated high-pitched scratchy “friction rub” is 100% specific for pericarditis.3 While chest x-ray may detect effusions larger than 250 cc, a bedside echocardiogram can detect as little as 20–50 cc of pericardial fluid3 and up to 60% of pericardial effusions.7 ECG with PR depression or ST changes that do not match anatomic regions, low voltage, and electrical alternans suggests a large pericardial effusion and should prompt evaluation for tamponade physiology. Classically, the ECG findings seen with pericarditis evolve through 4 stages:
- Diffuse concave upward ST-elevations (typically 2-4 mm) and PR segment depressions diffusely in all leads other than aVR and V1 which will show PR segment elevations and ST-segment depressions
- Normalization of ST and PR segments plus T-wave flattening
- Diffuse T-wave inversions, typically in the leads that previously had ST-segment elevation
- ECG normalizes or may have some persistent T-wave inversions2
Bloodwork is non-specific or sensitive, but may show leukocytosis, elevated ESR and CRP, while positive cardiac enzymes would indicate myocardial involvement.2,3,5,7
There is no specific work-up for Lyme disease in the ED. The Infectious Diseases Society of America (IDSA) supports a clinical diagnosis and subsequent treatment of erythema migrans.8 Serologic tests should only be performed 6-8 weeks into the suspected disease after antibodies have developed. The CDC recommends a 2-tier testing for Lyme Disease, which includes an initial enzyme immunoassay (EIA) such as enzyme-linked immunosorbent assay (ELISA) or immunofluorescence assay (IFA) followed by a Western blot. If the immunoassay is negative, the diagnosis of early disseminated or late Lyme disease is unlikely. If the immunoassay is positive, the Western blot should be performed and interpreted accordingly:8
Early disseminated Lyme disease: detectable IgM and IgG antibodies to B. burgdorferi. An isolated positive IgM Western blot may represent a false positive test. If there’s evidence of erythema migrans, the recommendation is to treat empirically and repeat testing in 3 weeks.
Late Lyme disease: IgG should be positive. IgM may or may not be positive and should not be used for diagnosis. Serology might be positive for months to years after infection.6,8
Although non-diagnostic, bloodwork may show leukocytosis, anemia, thrombocytopenia, ESR>30 mm/hr, elevated liver enzymes (notably γ-glutamyl transferase). In Lyme meningitis, CSF analysis will reveal pleocytosis and elevated protein, but CSF spirochete antibodies are not recommended.3,8 In Lyme mono-arthritis, joint effusion cryoglobulin may be increased 5-fold compared with serum.3,8
If the most common cardiac manifestation of Lyme is observed (first-degree heart block), admission may be warranted as patients may rapidly decompensate into second- and third-degree atrioventricular block, and some patients require a temporary pacemaker.2,7
Treatments
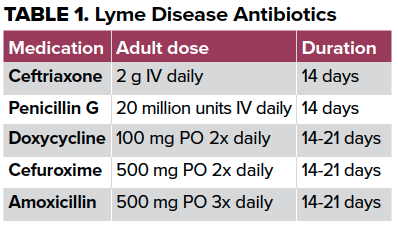
Treating the early manifestations of Lyme disease is important to prevent complications. Oral antibiotics (doxycycline, cefuroxime or amoxicillin) may be used for early localized disease or mild cardiac involvement, while intravenous antibiotics (ceftriaxone or penicillin G) are suggested for disseminated and more severe cardiac manifestations.1,2,3,7,8 Prophylactic use of antibiotics after a tick bite is controversial, but a one-time dose of 100 mg oral doxycycline for children and 200 mg for adults may be administered.8
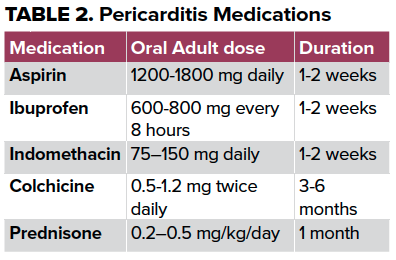
Acute pericarditis treatment with non-steroidal anti-inflammatories and colchicine should be started in the ED. Refractory pericarditis treatment include low to moderate doses of corticosteroids with taper and colchicine for at least 6 months.2,3,8 Patients who are stable, afebrile, without large pericardial effusions and reliable follow-up may be managed outpatient as most patients tend to recover within 3 weeks.7 Cases of pericarditis that are resistant to NSAIDs, colchicine and corticosteroids are extremely difficult to treat and may require pericardiectomy.7 Unless the patient presents with cardiac tamponade, ED pericardiocentesis is not recommended and should be performed by interventional cardiology.2,3
TAKE-HOME POINTS
- As with all undifferentiated patients in the ED, taking a good history is of utmost importance to diagnose both Lyme disease and pericarditis.
- Although there are no signs or symptoms specific for pericarditis, the diagnosis can be made if the patient has a constellation of symptoms including preceding illness, low-grade fever, dyspnea exacerbated by laying down, and pleuritic chest pain. ECG is helpful but unreliable and lab tests are not specific. An auscultated friction rub is very specific for pericarditis, yet it comes with environmental challenges in a busy ED.
- To diagnose a pericardial effusion, the single best tool we have in the ED is the ultrasound.
- Although not every patient with Lyme carditis requires hospital admission, even first-degree heart blocks can quickly decompensate into third-degree and the decision about disposition should be made with our consulting cardiologists.
- Treatment with NSAID and colchicine should not be delayed for suspected pericarditis.
- The same holds true for initiating antibiotic treatment for Lyme disease since delayed treatment can lead to progression of disease and confirmatory tests might take days to weeks to result.
REFERENCES
- Lyme Disease. CDC. https://www.cdc.gov/lyme/index.html. Published 2020. Accessed 202
- Zipes D, Braunwald E. Chapter 50: Pericardial Diseases. In: Braunwald's Heart Disease: a Textbook of Cardiovascular Medicine. 6th ed., Saunders, 2001. 1823-1876.
- Schaider J, Barkin A, Barkin R, Shayne P, Wolfe R, Hayden S, Rosen P. Rosen & Barkin’s 5-Minute Emergency Medicine Consult. 5th Wolters Kluwer Health/Lippincott Williams & Wilkins, c2015
- Haddad FA, Nadelman RB. Lyme disease and the heart. Front Biosci. 2003 Sep 1;8:s769-82. doi: 10.2741/1065. PMID: 12957829.
- Robinson ML, Kobayashi T, Higgins Y, Calkins H, Melia MT. Lyme carditis. Infect Dis Clin North Am. 2015 Jun;29(2):255-68. doi: 10.1016/j.idc.2015.02.003. PMID: 25999222.
- Branda JA, Aguero-Rosenfeld ME, Ferraro MJ, et al. 2-tiered antibody testing for early and late Lyme disease using only an immunoglobulin G blot with the addition of a VlsE band as the second-tier test. Clin Infect Dis 2010; 50:20.
- Jouriles, Nicholas J. Chapter 10: Myocardial and Pericardial Disease. In: Rosen's Emergency Medicine: Concepts and Clinical Practice: Volume 2, Mosby/Elsevier, 2010.
- Cameron DJ et al. Evidence assessments and guideline recommendations in Lyme disease: the clinical management of known tick bites, erythema migrans rashes and persistent disease. Expert Rev Anti Infect Therapy. Expert Rev Anti Infect Ther. 2014 12(9): 1103-35.



