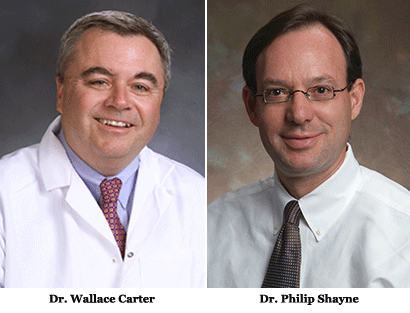
I recently had the opportunity to sit down with Drs. Wallace Carter, chair, and Philip Shayne, vice chair, of the Residency Review Committee (RRC) for emergency medicine. I asked these physician leaders about everything from their positions with the committee to their thoughts on the future of the field.
In addition to his role as chair of the RRC, Dr. Carter is the emergency medicine residency program director at New York Presbyterian Hospital. He graduated from the Ross School of Medicine and completed residency at the Bronx Municipal Hospital Center and St. Barnabas Hospital.
Dr. Shayne, vice chair of the EM-RRC, has been the program director at Emory since 1999 and also serves as the university's vice chair for education. He graduated from the University of Pennsylvania in 1981, the University of Illinois at Chicago College of Medicine in 1989, and the Cook County Hospital Emergency Medicine residency program in 1993. He is past president of the Council of Emergency Medicine Residency Directors (CORD), and is an American Board of Emergency Medicine (ABEM) oral boards examiner.
How would you describe the RRC to a PGY-I resident?
Carter: It is your training “safety net.” If your program has a 10-digit Accreditation Council for Graduate Medical Education (ACGME) program code, then it has undergone a rigorous evaluation process, including a site visit with accreditation specialists that is guided by very precise specialty requirements (which all residents should read at least once). Each specialty has its own RRC and specialty requirements. The great news is that residents are then free to choose a program based on personality, location, and practice type, and not worry if they are up to standard — the RRC has already done that for you.
Shayne: The ACGME is the non-governmental organization that has a mandate to accredit (approve) residencies and ensure they meet common and specialty requirements. Hospitals can't get funding to pay for residents unless the residency program is accredited. The ACGME has 27 specialty residency review committees comprised of mainly physicians in that specialty who maintain the requirements and ensure that residencies adhere to them. The ACGME is concerned about quality of education, resident wellness and safety, and the quality and safety of patient care.
What are you most proud of during your time on the RRC?
Carter: The last six years in the ACGME has been one of the most cataclysmic periods of change, next to the period around the Flexner Report. We are completely retooling the way we train physicians in this country. This new direction had tremendous potential to go badly. Instead, it went well, especially in emergency medicine, where our faculty and residents saw this as an incredible opportunity to embrace change and shape the future. As is the tradition of our specialty, EM became the change leaders within the ACGME.
Shayne: Not being assassinated (program directors don't like to be told how to do things). But seriously, it is an honor to be allowed to work with such a dedicated group, and I am proud of the expression of confidence from my peers when I was selected to be on the committee.
What is your best EMRA memory?
Carter: Passion and incredible energy. Whether it was Milestone creation or a program review, you knew that the residents knew how to bring their “A-game.” I was always nervous when I was paired with an EMRA resident for a program review because, invariably, they would find an issue I missed. To their credit, they were always most gracious about it. I learned early on in my tenure to never disagree with the resident.
Shayne: When I told the EMRA board that Emory didn't need a “residents' day” because every day was residents' day. They were too polite to tell me I was a self-righteous jerk.
What are your thoughts on the Milestones?
Carter: I am very excited about Milestones. Historically, evaluations were incredibly subjective. The evaluators were unsure what they should be evaluating, and the residents did not know on what they were being evaluated. For the first time, we have very clear ideas about what residents should look like by the time they graduate. The beauty of Milestones is that they need to be measured and validated. This hopefully begins to eliminate the evaluation card that says, “a great resident who is always smiling,” and replaces it with one that says, “a great resident who is always smiling who, during today's shift, was observed to complete a very difficult task that required team participation and advanced communication skills.” Can you see the potential?
Shayne: The Milestones are an interesting experiment. The Holy Grail has been to try and approve residencies by the quality of the physicians they train, as opposed to surrogate markers (e.g., number of ED patients in the hospital, the number of intubations by a resident, credentials of faculty). But it is very hard to measure competency or quality. The initial “core competency” experiment didn't work well; the Milestones are a way to get more concrete, detailed measurements of resident progress.
As the chair and vice chair of the RRC, what are your roles in the grand scheme of academic emergency medicine and GME?
Carter: As chair, I was incredibly lucky to be surrounded by nine superstars who could not wait to take on this challenge and make it perfect for our residents. The job of the chair and the committee is to be the GME community's “Switzerland.” We need to look at all of the competing needs and agendas of the various stakeholders and try to come to consensus, if possible, while being very aware that ultimately we must answer to our patients and residents.
Shayne: Wow, big question that could be answered in different ways. The RRC is the counterforce against the financial pressures and service burdens from the hospitals that employ residents. The committee needs to understand the specialty and the environment, and be both collaborative and firm in the interest of the residents. I guess, as chair, you get to set the tone. Vice chair gets to sit next to the guy who sets the tone.
Do you have a prediction for a major change from the ACGME in five years?
Carter: I think we will begin to see the very earliest benefits of changing to a system that requires data and is questing for outcome measurements. That will require a much longer time period to fully reveal itself, but — by then — we should have residents who are totally comfortable questioning every aspect of their training and thinking about how they can do it better.
Shayne: No fair – the Next Accreditation System (NAS) and the Milestones are once in 10- to 20-year seismic changes. The next five years should be spent organizing how the dust settles.
Do you have a prediction for a major change in emergency medicine within the next five years?
Carter: Change is coming; I just have no idea what form it will take. The ACA, the current economics of health care, and the increasing intrusion of accrediting bodies who falsely cloak so many of their mandates under the mantra of “safety and quality,” will require EM practitioners to be incredibly flexible and creative. Otherwise, these bureaucratic intrusions threaten to get between us and our patients and threaten our ability to care for every patient who comes through our doors, which is the cornerstone of emergency medicine.
Shayne: Well, the easy ones are that we are going to be busier, more crucial, and require even more flexibility in what we do. Hopefully, the EMRs will start fulfilling their promise of integrating decision rules into our practice to make it more efficient, safe, and economical. The big change for us, I think, will be cuts in residency funding. Everyone who has a current spot got in at the right time.
You are both program directors at your respective programs. What is most rewarding about your position as PD?
Carter: I think that a PD is a lot like being a great chef. At the start, you have all of these wonderful ingredients, but they are unformed and — for the most part — tasteless. At the end of the process, you have the most wonderful creation that you get to share with the world. Both processes require attention to detail, technical ability, and the stamina to survive in a very
hot “kitchen.” And both require you to break a few eggs.
Shayne: Watching residents grow and realize their potential. Residency is a very special time, during which you gain an incredible number of practical skills that allow you to use your knowledge for good. Residency also requires learning discipline, selflessness, balance, coping mechanisms, and professional demeanor. I love the end of June when we meet the interns-to-be — excited, scared, and mostly useless beside our experienced, weary, competent, and very ready senior residents. It makes our contribution to their development very tangible.
How has EMRA's presence on the RRC impacted residents?
Carter: While everything that is done at the ACGME is in service to our patients, residents are the end users of all of the accreditation rules and standards. They bring that unique perspective to all of our deliberations and are our “content experts.” We could not do our job without EMRA.
Shayne: It ensures that the decisions that the RRC makes, whether for the specialty requirements or concerning an individual program, are vetted from the residents' perspective. I think that we all have the residents' best interests at heart, but the rest of our perspectives can be compromised by our understanding and sympathy with the struggles of the medical systems, departments, programs, and program directors. The thing that makes me valuable — lots of firsthand experience in running a program — can also be a barrier, and it is great to have a fresh set of eyes. Interestingly, sometimes it is the resident member who is the most militant about raising expectations.
What is the best advice you can give to graduating EM residents?
Carter: Relax, and welcome to the best job in medicine. Enjoy the fact that every day you will have a meaningful impact on your patients; in many cases, it will be lifelong. Enjoy the fact that on a Monday night you can save someone's father, and the next afternoon you can be climbing a mountain or sailing. That does not exist in too many other specialties. Enjoy it!
Shayne: Enjoy the privileges and abilities that you have earned through your hard work. Enjoy that paycheck; you earned it. Enjoy having people thank you; you earned that. Enjoy how many jobs are available, how easy it is to relocate, and the respect that you get. You earned it. You have the ability to help someone in crisis every single time that you go to work; that is pretty cool, and you should enjoy it.