Dhimitri Nikolla, MSIV, Lake Erie College of Osteopathic Medicine, Erie, PA
Tyler Lewandowski, DO, Resident Physician Emergency Medicine, UPMC Hamot, Erie, PA
Introduction
Acute scrotal pain is a common complaint in the emergency department. Clinical signs and symptoms such as pain, tenderness, edema, and erythema can be present, but these symptoms overlap with a variety of other diagnoses. Therefore, it is often difficult to differentiate the benign from the emergent etiologies based on history and physical exam alone without the use of color-coded Doppler ultrasonography. As emergency physicians, we must rapidly and accurately assess patients with acute testicular symptoms, as testicular torsion is a fertility-threatening surgical emergency. There is utility in complementing clinical findings with color-coded Doppler ultrasonography in the assessment of patients with testicular torsion.
Testicular torsion is a fertility-threatening surgical emergency
Case
A 61-year-old male comes to the emergency department complaining of gradual onset of worsening right scrotal swelling. He first noticed the swelling about 1.5 weeks ago. There have been no fevers, chills, discharge, or dysuria. The pain is not exacerbated with coughing or sexual activity. His vital signs are normal. His right testicle is markedly enlarged when compared to the left. The testicle is tender to manipulation, but has no erythema or calor. Neither a Prehn sign nor a cremasteric reflex are present. There are no scrotal or penile skin lesions, no hernia, and a urinalysis is normal. A formal scrotal ultrasound is obtained, which reveals a large cystic lesion within the right scrotum, a moderately sized right hydrocele, and a small epididymal head cyst. There is no evidence of torsion (Image 1). The patient is safely discharged with instructions to follow up with an urologist as an outpatient in 3-5 days.
Discussion
Acute testicular pain can have multiple etiologies. Testicular torsion is the most significant and carries the greatest morbidity. It is no surprise that this is usually at the top of the list of conditions to rule out before discharging our patients. However, how effectively can we rule out a testicular torsion in the emergency department? Can it be done clinically, and what is the role of ultrasound?Although testicular torsion is a clinical diagnosis, the history and physical exam are more effective at ruling in the diagnosis than ruling it out. In a study of 90 patients <18 years old with either epididymitis, testicular torsion, or torsion of the appendix testis, a duration of symptoms <12 hours and nausea/vomiting were the most common historical features associated with testicular torsion, and were present in 69% and 31% of patients, respectively.1 However, 62% of patients with torsion of the appendix testes also had a symptom duration <12 hours, while 16% of patients with epididymitis had nausea/vomiting.1 As previously mentioned, this clinical overlap makes it difficult to distinguish testicular torsion from other acute scrotal pathologies.
Similarly, physical exam findings are not much better than historical features at differentiating the etiologies of acute scrotal pain.2 As seen in Table 1, specific findings on physical exam generally have poor negative likelihood ratios for ruling out testicular torsion, with the exclusion of the focal or localized findings.2 If only the history and physical exam were to be used to rule out the diagnosis, many testicular torsions would go undiagnosed.3 In a study looking at 209 emergency scrotal explorations, there were 82 cases of surgically-confirmed testicular torsion; in five of those cases (6%), the surgeon had not considered it the most likely diagnosis.3 Thus, the diagnosis would have been missed in those cases if no surgical scrotal explorations had been performed.
The Testicular Workup of Ischemia and Suspected Torsion (TWIST) study proposed a clinical scoring system that challenges the paradigm that history and physical cannot rule out testicular torsion.4 In this prospective study of 338 patients with acute scrotal pain, the scoring system was shown to have negative and positive predictive values of 100% for scores below 2, and above 5, respectively. The cited specificity was 97% and the sensitivity was reported at 54%.4 The scoring system (Table 2) may aid clinicians in the disposition of high- and low-risk patients without the need for color-coded Doppler ultrasonography, which is the current gold standard. However, the authors conclude the scoring system should be validated before we can apply it to our clinical practice.4 They also recommended that patients who fall between 2 and 5 on the scoring system should undergo Doppler ultrasound of the scrotum and testes.
While the aforementioned TWIST score has promise, color-coded Doppler ultrasonography is still the gold standard for assessment of testicular torsion. In a study of 236 patients with a clinical suspicion of testicular torsion, color-coded Doppler ultrasound had a sensitivity and specificity of 100% and 75.2%, and positive and negative predictive values of 80.4% and 100%, respectively.5 This strong negative predicative value makes color-coded Doppler ultrasonography the ideal test to rule out testicular torsion, and evidence supports its use at the bedside in the emergency department.
In a retrospective study of 36 patients with complaints of acute scrotal pain, bedside ultrasonography by the emergency physician coincided with confirmatory studies in 35 of the 36 patients.6 This agreement resulted in a sensitivity of 95% and a specificity of 94%.6 Nevertheless, there are rare case reports of testicular torsion with normal color Doppler sonography.7 Therefore, it is important to remember that test results should be used in conjunction with clinical gestalt and interpreted in the context of pretest probability.
Conclusion
Testicular torsion is a critical diagnosis in the emergency department. Although torsion should ideally be diagnosed clinically in order to expedite surgical intervention, history and physical are fallible and further risk stratification often requires the aid of color-coded Doppler ultrasonography. Although the recently derived TWIST score shows early promise for diagnosing or excluding testicular torsion, it requires further validation before it can be recommended for use in clinical practice.
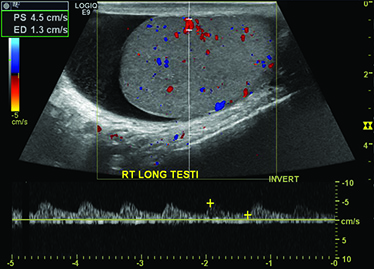
Image 1. Color Doppler sonogram of our patient's right testicle displaying normal arterial vascular flow and presence of a hydrocele. The ultrasound report also mentioned the presence of an epididymal cyst and a cyst within the testicle (not shown).
References
- Kadish HA, Bolte RG: A Retrospective Review of Pediatric Patients With Epididymitis, Testicular Torsion, and Torsion of Testicular Appendages. Pediatrics 102;73-76, 1998.
- Schmitz D, Safranek S. How useful is a physical exam in diagnosis testicular torsion? Journal of Family Practice 58;8: 433-434, 2009.
- Watkin NA, Reiger NA, Moisey CU: Is the conservative management of the acute scrotum justified on clinical grounds? British Journal of Urology 78;4; 623-627, 1996.
- Barbosa JA, Tiseo BC, Barayan GA, et al: Development and Initial Validation of a Scoring System to Diagnose Testicular Torsion in Children. The Journal of Urology 189: 1859-1864, 2013.
- Altinkilic B, Pilatz A, Weidner W: Detection of Normal Intratesticular Perfusion Using Color Coded Duplex Sonography Obviates Need for Scrotal Explor ation in Patients with Suspected Testicular Torsion. The Journal of Urology 189: 1853-1858, 2013.
- Blaivas M, Sierzenski P, Lambert M: Emergency Evaluation of Patients Presenting with Acute Scrotum Using Bedside Ultrasonography. Academic Emergency Medicine 8;1: 90-93, 2001.
- Allen TD, Elder JS: Shortcomings of Color Doppler Sonography in Diagnosis of Testicular Torsion. The Journal of Urology 154;4: 1508-1510, 1995.\




