Altered mental status (AMS) is a common presentation to the emergency department. Some studies suggest that mortality rate can be up to 1 in 10 for patients presenting with AMS.1
In the ED, an AMS patient requires a time-sensitive evaluation with primary survey — ABCDE: Airway, Breathing, Circulation, Disability, and Exposure, adding F for fingerstick glucose and initial vitals.1,2 After this initial assessment, a history and physical examination will allow you to evaluate for other causes. The differential diagnoses could be categorized as: primary central nervous system (CNS), metabolic, toxicologic, infectious, or other.1,2
Hyperviscosity syndrome belongs in the "other" category. It classically presents as a triad of neurological deficits, visual disturbances, and mucosal bleeding. It is also associated with blood dyscrasias such as erythrocytosis, leukocytosis, or thrombocytosis.3 It is a hematologic-oncologic emergency given that increased plasma viscosity slows blood flow, causing hypoperfusion of tissues.3
Case
A 48-year-old man with a history of hypertension and recently diagnosed bilateral lower extremity deep vein thrombosis presented to the ED via emergency medical service. A family member called EMS when the man became minimally responsive during the day. The patient was taking an anticoagulant.
On initial evaluation, the patient was oriented to self and place but appeared confused and lethargic. He was minimally responsive to questions, speaking slowly, and unable to provide a history.
Initial vitals were blood pressure 150/92; pulse 105 bpm; respiratory rate 22; O2 saturation 97% on room air; and temperature 98.8 degrees Fahrenheit. The patient was empirically treated with D50. Physical exam was remarkable for ill appearance, dry mucous membranes, poor skin turgor, disorientation, and inability to follow commands.
Family members reported that the patient had been behaving unusually for the past month and drinking alcohol more than usual after the death of a sibling. Two weeks prior to presentation, he had complained of bilateral leg pain, at which point he was diagnosed with bilateral deep vein thrombosis and started on apixaban. One week prior to presentation, the patient felt nauseous and lightheaded, and family members took him to a hospital. He was diagnosed with decreased renal function and discharged after being managed with diuretics. One day prior to his presentation to our ED, a family member noticed that the patient appeared dehydrated with dry mucous membranes, was speaking incoherently, and fell after standing up.
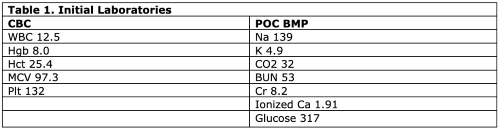
Initial lab results (Table 1) showed normocytic anemia, thrombocytopenia, elevated ionized calcium, and kidney injury.
A non-contrast head CT scan did not show signs of hemorrhage, edema, or tumors. However, chest, abdomen and pelvis CT scans did show evidence of bony lesion at T11 vertebral body (Image 1).
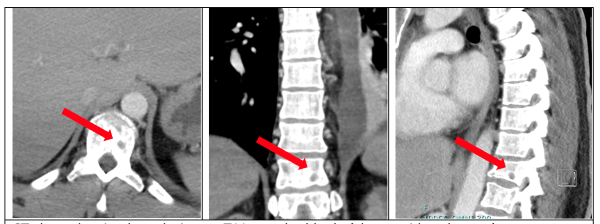 Figure 1. CT scan showing bony lesion
Figure 1. CT scan showing bony lesion
The patient was admitted to the medical ICU for close monitoring of altered mental status. Given his elevated BUN and creatinine, there was a concern for acute renal failure contributing to AMS and a likely requirement of emergent hemodialysis. The nephrology team agreed with beginning emergent hemodialysis and added a new differential of blood dyscrasia because of elevated total serum protein of 16.8.
Additional labs showed the patient had an elevated protein gap (or gamma gap, the difference between total serum protein and albumin) of 14.7, which raised the concern for hyperviscosity syndrome.
Hematology service recommended aggressive IV fluid hydration while preparing for urgent plasmapheresis. The patient promptly received plasmapheresis, which improved his mental status. He later received hemodialysis, which improved his renal failure.
The patient was subsequently diagnosed with multiple myeloma as the cause for hypercalcemia, requiring a total of 6 sessions of plasmapheresis and 2 sessions of hemodialysis. Chemotherapy was initiated. The patient was discharged after 40 days at the hospital.
Discussion
This case was an atypical presentation of hyperviscosity syndrome, given that initial presentation was AMS alone as opposed to the classic triad of neurological deficits, visual disturbances, and mucosal bleeding. Initial management was further complicated by frequent clotting of blood samples and limited amount of information from the patient’s past medical history.
However, a tool that showed to be useful was the total serum protein, which is consistent with paraproteinemia most commonly caused by monoclonal gammopathies.4 This patient presented with hyperCalcemia, Renal failure, Anemia, and Bony lytic lesions (features collectively known together as CRAB), which was concerning for multiple myeloma. The protein or gamma gap is a useful tool for multiple myeloma diagnosis because it has been shown to be a quick assessment of disease burden and treatment response.5 Although the gold standard for diagnosis is serum and urine protein electrophoresis, the turnaround time is 3 to 7 days. In case of emergent plasmapheresis, it is imperative to not delay treatment.5
Initial treatment of hyperviscosity includes consulting the hematology-oncology team for further evaluation and emergent plasmapheresis.6,7 While plasmapheresis may reduce viscosity by 30-50%, it will not treat the underlying disorder, and patients will be concomitantly started on chemotherapy.6,7 Chemotherapy is mostly directed toward symptom resolution or improvement rather than viscosity measurement itself because patients may have symptom resolution with an elevated viscosity.3
As patients with hyperviscosity syndrome are usually dehydrated, hydration with 1-2 liters of normal saline while awaiting plasma exchange is common practice.3 Another temporizing measure, especially if plasma exchange is unavailable, is phlebotomy by extracting 1-2 units of blood while concurrently replacing it with normal saline.3 However, this treatment is generally reserved for severe cases when patients present with coma or seizures.3
Conclusion
Altered mental status is a common presentation that requires a time-sensitive evaluation, given its mortality rate.1 Although presentation for AMS could be addressed under broad categories such as structural CNS, metabolic, infectious, or toxicologic, an additional category worth considering is blood derangements, such as blood dyscrasias.1,2 Our case demonstrated the difficulties of a time-sensitive evaluation in a patient with hyperviscosity syndrome.
Important steps to determine patient management include recognizing the CRAB features suggestive of multiple myeloma and determining the gamma gap. In our case, this directed management toward immediate hydration and plasma exchange as temporizing measures. This treatment is meant to improve symptoms but not necessarily tend to the viscosity, although an argument can be made for assessing treatment response via the gamma gap.5
Take-Home Points
- Consider blood dyscrasias when evaluating altered mental status.
- Hyperproteinemia is mainly caused by monoclonal gammopathy but might be seen in inflammatory diseases. Consider multiple myeloma as a differential for an elevated protein or gamma gap.
- Hyperviscosity syndrome is a hematologic-oncologic emergency. Give intravenous fluids as patients will be dehydrated. In cases of coma or seizure, consider phlebotomy if unable to promptly perform plasma exchange.
- Patients will require admission for further management, which may require multiple sessions of plasmapheresis and testing to determine the etiology that will ultimately guide treatment.
References
- Lahue SC, Douglas VC. Approach to Altered Mental Status and Inpatient Delirium. Neurol Clin. 2022;40(1):45–57.
- Alvarez A, Morrissey T. Approach to Altered Mental Status. Clerkship Directors in Emergency Medicine. Published 2019.
- Rogers AP, Estes M. Hyperviscosity Syndrome. StatPearls. Published online March 13, 2023. Accessed October 22, 2023.
- Tate JR. The Paraprotein-an Enduring Biomarker. Clin Biochem Rev. 40(1):2019-2024.
- Dupuis MM, Paul B, Loitsch G, et al. Gamma Gap: A Point-of-Care Test That Correlates With Disease Burden and Treatment Response in Multiple Myeloma. JCO Oncol Pract. 2020;16(8):e751-e757.
- Gertz MA. Acute hyperviscosity: syndromes and management. Blood. 2018;132(13):1379-1385.
- Stone MJ, Bogen SA. Evidence-based focused review Evidence-based focused review of management of hyperviscosity syndrome. Blood. 2012;119(10):2205-8.



