Initial Presentation
A 10-year-old girl presented to the emergency department with 10 days of fever and sore throat, 1 day of arthralgias, and a lower extremity rash.
Approximately 1 week prior to presentation, the patient’s father and brother had tested positive for strep throat. Due to the patient’s ongoing symptoms, her primary care provider treated her empirically with a course of azithromycin, which the patient started 4 days prior to presentation. While her fever and sore throat improved after starting the antibiotic, they did not resolve, and she developed arthralgias and a lower extremity rash.
In the emergency department, the patient was afebrile with normal vital signs. On exam she had perioral excoriations, mild tonsillar erythema, bilateral knee swelling with mild tenderness, an erythematous petechial rash on her abdomen, and 5-10 millimeter palpable purpura on bilateral lower extremities with excoriation (Image 1). Laboratory tests were notable for mild leukocytosis (9.57 K/UL, ref. range), elevated erythrocyte sedimentation rate (62 MM/H, ref. range 0-12 MM/H), and elevated C-Reactive protein (5.7 MG/DL, ref. range <0.5 MG/DL). Her anti-streptolysin O titer was elevated to 3620 IU/mL (ref range 0-640 IU/mL). Urinalysis was notable for trace proteinuria but was concentrated.

Image 1: Palpable purpura
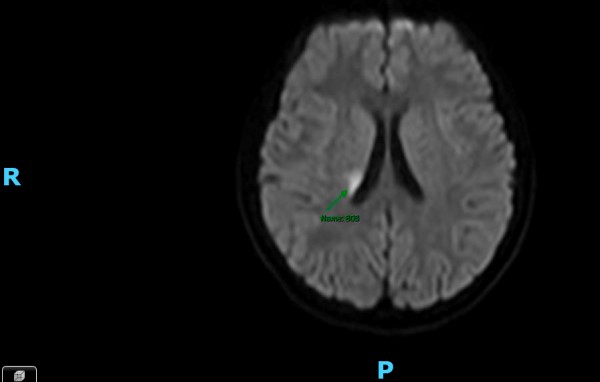
Image 2: MRI
The patient was admitted to the hospital overnight for monitoring. She was clinically diagnosed with Henoch-Schönlein purpura (HSP) immunoglobulin A vasculitis (IgAV) and peri-oral impetigo, for which she was prescribed a 10-day course of cephalexin. Additional recommendations included outpatient monitoring of blood pressure and repeat urinalysis to assess for secondary effects of IgAV.
Second presentation
Five days after discharge, the patient re-presented to the ED with left-sided tingling and weakness. She also noted that she developed an achy feeling in her torso and back that she continued to feel with deep breathing. She additionally endorsed persistent diffuse abdominal pain, nausea, and vomiting that had been occurring since her discharge from the hospital.
In the ED, she had diastolic hypertension (118/91) with otherwise normal vital signs. Her skin exam was notable for erythematous patches without clear borders on her bilateral wrists and forearms and light purple macules scattered on bilateral legs that had improved from purpura at her prior presentation. Her neurological exam was notable for left patellar hyperreflexia, 4 to 5 beats of left ankle clonus, and decreased pinprick sensation over her left lower extremity.
Pediatric neurology was consulted. Magnetic resonance venography of the brain and spine revealed diffuse restriction in the right frontoparietal white matter extending to the right putamen/globus pallidus with acute/subacute infarction, for which she was started on baby Aspirin. General pediatrics admitted the patient to their service.
Pediatric neurology, nephrology, dermatology, rheumatology, cardiology, and genetics (due to concern for carrier trait of familial Mediterranean fever) were consulted. A skin biopsy was diagnostic for IgAV.
Rheumatology labs were unremarkable, and genetic testing for familial Mediterranean fever was negative. Due to concern for vasculitis stroke, the patient received 125 mg of methylprednisolone every 6 hours for 3 days. She was ultimately discharged with daily 20 mg prednisone and rheumatology follow-up.
At an outpatient neurology follow-up 77 days after discharge, the patient’s mother reported with concern for mild residual cognitive deficits (difficulty with measurements) and left-hand drooping while playing piano. The patient was otherwise doing well and had a full return of strength, sensation, and energy levels.
Discussion
IgAV is the most common form of present vasculitis in children,1 accounting for an estimated 58% of primary vasculitis in children,2 and with an estimated annual incidence of approximately 10-20 cases per 100,000.3,4
Immunoglobulin A (IgA) is an immunoglobulin present in mucosal tissues. While the exact pathophysiology of IgAV is unknown, it is thought to be related to abnormal glycosylation of the hinge region of IgA1, which serves as an antigen to autoantibodies that then form immune complex.1,5
Diagnosis is clinical and includes the presence of palpable purpura with at least 1 of the following: a biopsy demonstrating IgA deposition with gastrointestinal (abdominal pain), musculoskeletal (arthralgias or arthritis), or renal (hematuria or proteinuria) involvement.3
Less commonly, patients with IgAV will present with involvement of the neurologic system, cardiopulmonary system, or scrotum.5
The patient in this case met several criteria: biopsy, arthralgias, and trace proteinuria.
Treatment varies based on the severity of organ system involvement, but it is typically supportive.2
Interestingly, infection — particularly infection with streptococcus bacteria — has been identified as a common trigger for the development of IgAV.2 This was seen in this particular case. In a study of 1,200 pediatric cases of IgAV in China, potential infection was present in almost 51% of cases, with streptococcal infection being present in approximately 17% of cases.6 Streptococcal involvement was found to be even higher (18.9% of cases) in a study examining more than 2,000 cases of IgAV in Chinese children.2
Central nervous system involvement in IgAV can occur; however, it is considered rare and only occurs in 1-8% of pediatric cases.7 CNS involvement has been reported to include headaches, seizures, focal neurologic deficits, and posterior reversible encephalopathy.7,8
In one study that reviewed all CNS-involved HSP cases from 1969 to 2009, 44 of the 54 patients were younger than 20 years old.9 Thirty-five of these patients had neuroimaging, which had a wide array of findings: vascular lesions involving 2 or more vessels, intracerebral hemorrhage, brain edema, and thrombosis of the superior sagittal sinus.
Interestingly, the patient in this case had neither any vascular abnormality nor thrombosis on the MRI/MRV. As there is a varying presentation of CNS involvement in HSP, this makes the diagnosis challenging.
Ideal management of CNS involvement in HSP has not been fully elucidated. Steroids and cyclophosphamide are reasonable choices in patients with cerebral lesions. Additional rheumatologic testing is often performed, as other vasculidities are more common to have CNS manifestations than HSP. 9 Consider ANA and ANCA testing in these patients.
Conclusion
The general consensus for patients with HSP is that the majority of morbidity results from renal involvement. While HSP is relatively easy to diagnose, this case demonstrates that a thorough neurologic examination is prudent so as not to miss any CNS involvement, which is more variable. CNS involvement, while rare, can also lead to morbidity.
This case was also complicated by a likely incorrectly treated streptococcal infection. Azithromycin was chosen due to family preference as the patient’s parents had penicillin allergies. Fortunately, this particular patient had a good outcome with minimal neurologic sequelae.
References
- Oni L, Sampath S. Childhood IgA Vasculitis (Henoch Schonlein Purpura)—Advances and Knowledge Gaps. Front Pediatr. 2019;7. Accessed May 5, 2023. https://www.frontiersin.org/articles/10.3389/fped.2019.00257
- Fan GZ, Li RX, Jiang Q, et al. Streptococcal infection in childhood Henoch-Schönlein purpura: a 5-year retrospective study from a single tertiary medical center in China, 2015–2019. Pediatr Rheumatol. 2021;19(1):79. doi:10.1186/s12969-021-00569-3
- Leung AKC, Barankin B, Leong KF. Henoch-Schönlein Purpura in Children: An Updated Review. Curr Pediatr Rev. 2020;16(4):265-276. doi:10.2174/1573396316666200508104708
- Gardner-Medwin JMM, Dolezalova P, Cummins C, Southwood TR. Incidence of Henoch-Schönlein purpura, Kawasaki disease, and rare vasculitides in children of different ethnic origins. Lancet Lond Engl. 2002;360(9341):1197-1202. doi:10.1016/S0140-6736(02)11279-7
- Du L, Wang P, Liu C, Li S, Yue S, Yang Y. Multisystemic manifestations of IgA vasculitis. Clin Rheumatol. 2021;40(1):43-52. doi:10.1007/s10067-020-05166-5
- Wang JJ, Xu Y, Liu FF, et al. Association of the infectious triggers with childhood Henoch–Schonlein purpura in Anhui province, China. J Infect Public Health. 2020;13(1):110-117. doi:10.1016/j.jiph.2019.07.004
- Iannetti L, Zito R, Bruschi S, et al. Recent Understanding on Diagnosis and Management of Central Nervous System Vasculitis in Children. Clin Dev Immunol. 2012;2012:698327. doi:10.1155/2012/698327
- Zhang S, Yuan D, Tan G. Neurological Involvement in Primary Systemic Vasculitis. Front Neurol. 2019;10:430. doi:10.3389/fneur.2019.00430
- Garzoni L, Vanoni F, Rizzi M, et al. Nervous system dysfunction in Henoch-Schonlein syndrome: systematic review of the literature. Rheumatol Oxf Engl. 2009;48(12):1524-1529. doi:10.1093/rheumatology/kep282



