How Federal Funding for CPR and AED Training Can Save Lives in Out-of-Hospital Cardiac Arrest
Most cardiac arrest cases in the United States occur outside of the hospital, yet bystanders intervene less than half of the time. Survival rates from out-of-hospital cardiac arrest (OHCA) are disparate globally: less than 10% in the U.S., and in China they are as low as 1.2% annually, for example.
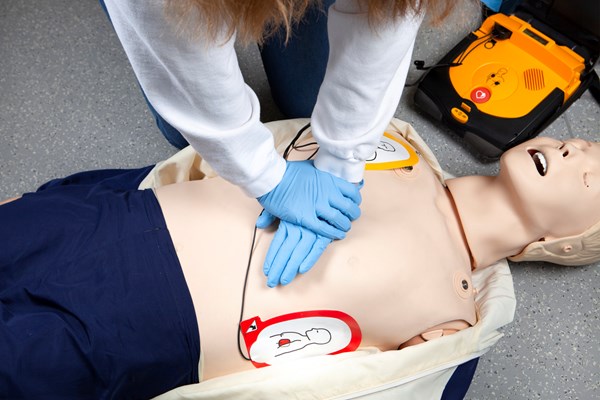
In 2018, China enacted legislation to promote the implementation of cardiopulmonary resuscitation (CPR) and automated external defibrillators (AED) training for the public and clarify the legal responsibility of dispatchers and bystanders in a few pilot cities. This study evaluates the impact of the 2010 legislation on OHCA in one pilot city, Shenzen. Using EMS data, researchers performed an interrupted time-series analysis of OHCA outcomes between 2010 and 2022.
They also evaluated changes in rates of CPR and AED use in witnessed, adult OHCAs: 7,858 OHCAs occurred pre-legislation, and only 5,892 OHCAs post-legislation. Bystander CPR rose significantly (4.10% to 18.73%), as did dispatcher instruction during CPR (3.12% to 5.29%). AED administration by EMS decreased significantly (4.07% to 0.96%) and the time between collapse, EMS call, and EMS contact with the patient all decreased, though the decrease was small. Prehospital return of spontaneous circulation (ROSC) increased significantly (0.92% to 7.21%), with improved survival at arrival to the hospital and discharge.
Controlling for confounders, likelihood of bystander CPR/AED use, achieving ROSC, and surviving the hospital were all higher post-legislation. This study shows that legislation mandating bystander CPR and AED training improves OHCA survival and that the results are sustainable over time. However, this study does not provide data on neurologic outcomes, information on the bystanders, or the quality of CPR.
This research aligns with U.S. studies showing increased CPR and AED use in states with protective laws. Currently, 40 states and D.C. require CPR education before high school graduation, which improves outcomes. However, these laws are state-specific, and no state or federal legislation exists that mandates the training of individuals outside of school settings.
EM TAKEAWAY
The evidence is clear: to reduce the burden of OHCA and ultimately save lives, federal legislation and substantial funding must be prioritized to expand CPR and AED training nationwide beyond schools and extend to workplaces, community centers, and religious institutions. The time to act is now.
ABSTRACT
Li S, Qin C, Zhang H, et al. Survival After Out-of-Hospital Cardiac Arrest Before and After Legislation for Bystander CPR. JAMA Netw Open. 2024;7(4):e247909.
Abstract importance The lack of evidence-based implementation strategies is a major contributor to increasing mortality due to out-of-hospital cardiac arrest (OHCA) in developing countries with limited resources.
Objective: To evaluate whether the implementation of legislation is associated with increased bystander cardiopulmonary resuscitation (CPR) and automated external defibrillator (AED) use and improved clinical outcomes for patients experiencing OHCA and to provide policy implications for low-income and middle-income settings.
Design, Setting, and Participants: This observational cohort study analyzed a prospective city registry of patients with bystander-witnessed OHCA between January 1, 2010, and December 31, 2022. The Emergency Medical Aid Act was implemented in Shenzhen, China, on October 1, 2018. An interrupted time-series analysis was used to assess changes in outcomes before and after the law. Data analysis was performed from May to October 2023.
Exposure: The Emergency Medical Aid Act stipulated the use of AEDs and CPR training for the public and provided clear legal guidance for OHCA rescuing.
Main Outcomes and Measures: The primary outcomes were rates of bystander-initiated CPR and use of AEDs. Secondary outcomes were rates of prehospital return of spontaneous circulation (ROSC), survival to arrival at the hospital, and survival at discharge.
Results: A total of 13,751 patients with OHCA (median [IQR] age, 59 [43-76] years; 10,011 men [72.83%]) were included, with 7858 OHCAs occurring during the prelegislation period (January 1, 2010, to September 30, 2018) and 5893 OHCAs occurring during the postlegislation period (October 1, 2018, to December 31, 2022). The rates of bystander-initiated CPR (320 patients [4.10%] vs 1103 patients [18.73%]) and AED use (214 patients [4.12%] vs 182 patients [5.29%]) increased significantly after legislation implementation vs rates before the legislation. Rates of prehospital ROSC (72 patients [0.92%] vs 425 patients [7.21%]), survival to arrival at the hospital (68 patients [0.87%] vs 321 patients [5.45%]), and survival at discharge (44 patients [0.56%] vs 165 patients [2.80%]) were significantly increased during the postlegislation period. Interrupted time-series models demonstrated a significant slope change in the rates of all outcomes.
Conclusions and Relevance: These findings suggest that implementation of the Emergency Medical Aid Act in China was associated with increased rates of CPR and public AED use and improved survival of patients with OHCA. The use of a systemwide approach to enact resuscitation initiatives and provide legal support may reduce the burden of OHCA in low-income and middle-income settings.
EMRA + PolicyRx Health Policy Journal Club: A collaboration between Policy Prescriptions and EMRA
 As emergency physicians, we care for all members of society, and as such have a unique vantage point on the state of health care. What we find frustrating in our EDs - such as inadequate social services, the dearth of primary care physicians, and the lack of mental health services - are universal problems. As EM residents and fellows, we learn the management of myocardial infarctions and traumas, and how to intubate, but we are not taught how health policy affects all aspects of our experience in the ED. Furthermore, given our unique position in the health care system, we have an incredible opportunity to advocate for our patients, for society, and for physicians. Yet, with so many competing interests vying for our conference education time, advocacy is often not included in the curricula. This is the gap this initiative aims to fill. Each month, you will see a review of a new health policy article and how it is applicable to emergency physicians.
As emergency physicians, we care for all members of society, and as such have a unique vantage point on the state of health care. What we find frustrating in our EDs - such as inadequate social services, the dearth of primary care physicians, and the lack of mental health services - are universal problems. As EM residents and fellows, we learn the management of myocardial infarctions and traumas, and how to intubate, but we are not taught how health policy affects all aspects of our experience in the ED. Furthermore, given our unique position in the health care system, we have an incredible opportunity to advocate for our patients, for society, and for physicians. Yet, with so many competing interests vying for our conference education time, advocacy is often not included in the curricula. This is the gap this initiative aims to fill. Each month, you will see a review of a new health policy article and how it is applicable to emergency physicians.