Community paramedicine and mobile integrated healthcare are forming a new paradigm.
Using paramedics to evaluate and treat medically complex elderly patients in the home setting could have wide-reaching implications for health management, cost of care, and patient satisfaction. This article will examine the effect of TANDEM365, A home-based community paramedicine program (HBCP) on emergency department utilization, diagnostics and administered procedures, rate of transport and admission, and hospital length of stay.
TANDEM365 is a highly integrated, mobile healthcare organization partnered with a private insurance payer, Priority Health, that provides comprehensive solutions for geriatric patients. Care is provided by skilled, community-integrated paramedics, nurses, and social workers. Utilizing integrated paramedic care visits, TANDEM365 focuses on performing in-home urgent assessments during which patients are evaluated, medications are given, and multi-specialty care is coordinated.1 The program has since transformed into a community health system partner; hospital systems and insurance payers refer patients to TANDEM based on age, comorbidities, utilization, and projected life expectancy. Since its creation in 2014, TANDEM365 has treated more than 2800 patients.
METHODS
This was a retrospective cohort analysis of elderly patients (>65 years) who triggered emergency medical services (EMS) dispatch with urgent medical calls with one EMS agency involved over a 2-year period (2019-2020) within the Grand Rapids, Michigan metropolitan area. The institutional review board of Spectrum Health Hospital in Grand Rapids approved the study. Data from 2019 and 2020 were considered separately due to the unforeseen effect the coronavirus (COVID-19) pandemic had in 2020. HBCP members were compared to non-members (control group) in terms of demographics, presenting complaints, prehospital inventions, transport to 2 emergency departments (Spectrum Health Butterworth and Blodgett ED), length of hospital stay (LOS), and in-patient medical costs. A total of 1,419 unique HBCP members were enrolled during the study period. The primary outcome consisted of emergency department utilization compared to control with secondary outcomes consisting of admission percentage, in-patient length of stay, mortality, and subsequent total cost of care.
For both populations, we calculated the percentage of patients who were transported to the ED and subsequent length of stay. For HBCP members, we also analyzed the proportion of those patients who were evaluated in the home via urgent assessment and not transported to the emergency department. We then calculated their probability of presenting to the emergency department within 1 day of in-home evaluation. Comparisons between categorical variables were evaluated using the Chi-square test. P-values of <0.05 were considered statistically significant.
RESULTS
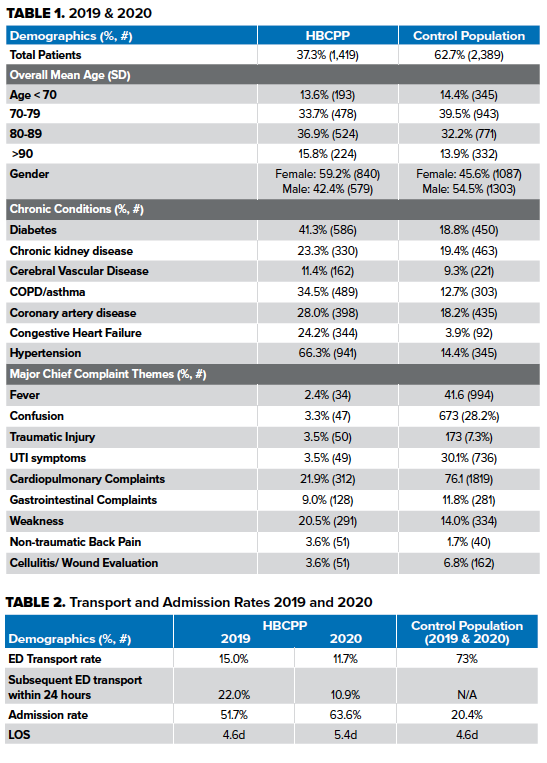
During the 2-year study period, there were 3808 unique EMS calls from elderly patients with high acuity conditions including fever, altered mental status, fall, dysuria, cardio-pulmonary complaints, fatigue or weakness, abdominal pain, back pain, hypertension, cellulitis, and anxiety. Demographic data as well as pertinent past medical history is compared in Table 1. In 2019 and 2020, a total of 1419 urgent assessment calls (37.3%) were from distinct HBCP members. Of this, 2389 (62.7%) were traditional EMS calls and served as our control. In terms of age, the mean age of the HBCP population was younger but within 1 SD (77.6 vs. 79.64).
Increased Medical Complexity
In both years as described, patients in the HBCP had increased medical comorbidities compared to the control population (Table 1): hypertension (66.3% vs. 47.5%), diabetes mellitus (41.3% vs. 18.8%), congestive heart failure (24.2% vs. 3.9%), and chronic obstructive pulmonary disease or asthma (34.5% vs. 12.7%).
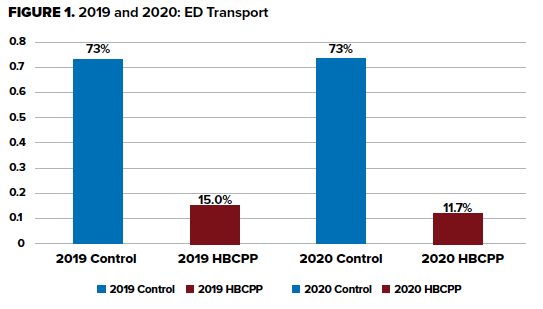
In 2019 HBCP members had reduced ED transport compared to control (15.0% vs. 73%)(p<0.001) with higher admission rates (51.7% vs. 20.4%). Moreover, the patients within the HBCPP had an identical admission LOS (4.6d vs. 4.6d) (p<0.001). During the first year of the COVID-19 global pandemic, 2020, HBCP patients continued to have reduced ED transport (11.7% vs. 73%) with an increased admission rate of 63.6%, an 18.7% increase from the previous year. Additionally, patients in 2020 also had an increased LOS of 5.44, a 0.48 day increase.
Emergency Department and Hospital Utilization
Our primary outcome was the comparison of ED utilization rates of the HBCP program compared to control. Furthermore, we were interested in the ED utilization percentage and timing of those HBCP patients initially evaluated and treated at home and not transported. HBCP patients not transported to the ED had subsequent ED evaluation rates within 24 hours of assessment of 22.0% vs. 10.9% (2019 vs. 2020). In terms of discharge disposition, 2019 HBCP patients required increased skilled nursing facilities compared to control population (35% vs. 20%), reduced discharge to home (23% vs. 43%), and identical mortality rates (3% vs. 3%).
Diagnostics and Administered Therapy
Notably, 25% of HBCPP patients who received a 12-lead ECG were transported to the ED vs. 99.4% of the control population. Furthermore, as we analyze IV fluid administration, 55.6% of HBCP patients who received IV fluids were transported to the emergency department vs. 100% (n=539) in the control population.
DISCUSSION
The Grand Rapids metropolitan area and specifically Kent County consists of a population of nearly 650,000 people with an annual call volume of 56,000 EMS runs, and utilizes a mix of 3 private BLS and ALS ambulance providers (AMR, Rockford, and Life-EMS) transporting patients to three 9-1-1 receiving emergency departments. Roeper and colleagues commented that certain Medicare population patients experienced non-emergent chief complaints and were better suited from a patient's satisfaction, quality, and cost of care, to be treated at home by an HBCP. They further contended that approximately 15% of Medicare patients transported to the ED were non-emergent or primary care treatable, costing about $1 billion to the health system per year.2 During the study years of 2019-2020, TANDEM365 HBCP reduced ED utilization (Figure 1) of high-risk and medically complex elderly patients by nearly 60% compared to traditional EMS. Our data is comparable to Bennet and colleagues, who described similar community paramedicine program metrics in a rural South Carolina EMS system that estimated 42% of EMS calls were non-urgent issues with the reduction of ED visits by 58.7% and decreasing in-patient visits by 69%.3
From year to year, at initial patient assessment, the HBCP reduced its ED transport by nearly 20%. Furthermore, the program reduced its subsequent 24-hour emergency department utilization by nearly 50% (22.0% vs. 10.9%). We attribute the decreased emergency department transport and re-utilization rates at 24 hours in part to key interventions made as a result of the initial 2019 data. This initial data suggested that patients had high ED utilization rates after not being transported. Nurse navigators reached out to patients within 24 hours after a home health assessment to discuss follow-up, which included primary care visits, sub-specialty outreach, and behavioral health or social service referrals. This is consistent with Nejtek and colleagues, who described a successful mobile integrated healthcare program that relied on patients and team members possessing a joint partnership to engage in navigational assistance and proactively assists patients seeking health resources outside of the ED.4
With the knowledge that the HBCP patients possessed more comorbidities at baseline (Table 1) this may also suggest the HBCP not only reduced emergency department utilization but also optimized it because EMS only transported those patients who truly warranted ED evaluation. Furthermore, this could suggest the triage and subsequent treatment performed by the community paramedics of this medically complex population is effective. One could also contend that the increased length of stay associated with the 2020 HBCP program was due to these patients who were initially treated at home, progressing in their illness, and thus were more appropriate to be evaluated (and subsequently admitted) in the traditional healthcare setting. However, as this study occurred during the COVID-19 pandemic with historically lower ED volumes, we cannot state with a degree of certainty the number of patients who were hesitant about emergency department evaluation, but rather delayed their presentation out of fear of contracting the virus. One piece of evidence that adds weight to this theory is that upon ED evaluation in 2020, HBCP patients were sicker, as suggested by the 19% increased HBCPP admission rates (63.6% vs. 51.7%) with an increased hospital length of stay of nearly half a day. Of note, patient mortality was the same as control at a rate of 3%, suggesting this program did not lead to increased mortality. Abrashkin and colleagues also identified in their community paramedicine program their members had higher admission rates of patients they transported than control (82.2% vs. 68.9%).5,6
Cost savings can be a difficult metric, given the many ways to calculate it. Stanhope and colleagues described a previous example of a Grand Rapids home-based primary community care model that described short-term increased costs upon entry to the program and substantial savings at the patient’s end-of-life. Authors estimated cost savings of $14,446 per member.7 The average claim for our control population (nearly 2,400 patients admitted in 2019) was $7,517.84. Using this estimate with the corresponding 2019 and 2020 admission percentages of the HBCP with those patients within the program who were not transported to the emergency department, the estimated and potential cost savings for the healthcare system excluding EMS was in the millions of dollars ($1.9 million to $3.2 million).
Limitations
Limitations of our study include limited ability to evaluate the true effect of COVID-19 on the program and its members. While HBCPs reduce ED utilization, it is difficult to tell the impact of COVID-19 stay-at-home orders and their effect on patient attitudes and decisions. In addition, the true cost savings are difficult to evaluate in terms of the average cost saved with EMS savings. In addition, lack of universal and consistent documentation in the prehospital setting of terms of chief complaints in the HBCP may lead to under-estimation of presenting complaints. Finally, it is difficult to determine whether a patient’s initial reason for in-home urgent assessment was the same reason for their subsequent ED visit. Finally, while patients were encouraged to call the TANDEM365 staff with any acute medical needs, it is possible patients utilized traditional 9-1-1 services with transport to an emergency department not within our study.
CONCLUSIONS
Our home-based community paramedicine program was started as a solution for at-risk seniors who have difficulty navigating the healthcare system to get the care they need and maintain their independence at home. These results suggest that the HBCPs reduced ED utilization during the study years of 2019-2020 with no increase in mortality.
In addition, it is likely this program saved significant money to the health system through optimized utilization of hospital admission. Further research into the safety and expansion of such programs will be informative on the large-scale generalizability of such programs.
Furthermore, large data sets and predictive analytics will empower mobile integrated health networks to better determine the need for transport based on patients’ comorbidities, symptoms, vital signs, response to prehospital treatment, and predicted re-utilization.
References
- TANDEM365. “Our Services.” https://tandem365.com/our-services/ 27 June 2021.
- Roeper et al. Mobile Integrated Healthcare Intervention and Impact Analysis with a Medicare Advantage Population. Population Health Management 2018;21(5):349-56. (Number 27 from Systematic Review)
- Bennett et al. Community Paramedicine Applied in a Rural Community. The Journal of Rural Health 2018;24:s39-s47.
- Nejtek at al. A pilot mobile integrated healthcare program for frequent utilizers of emergency department services. American Journal of Emergency Medicine 2017; 35:1702-5.
- Abrashkin et al. Providing Acute Care at Home: Community Paramedics Enhance an Advanced Illness Management Program - Preliminary Data. JAGS 2016;64:2572-6
- Mattke et al. Medicare Home Visit Program Associated With Fewer Hospital And Nursing Home Admission, Increased Office Visits. Health Affairs 2015. 34(12):2138-2146.
- Stanhope et al. The effects of home-based primary care on Medicare costs at Spectrum Health/Priority Health (Grand Rapids, MI, USA) from 2012-present: a matched cohort study. BMC Health Services Research 2018. 18:161.



