Direct oral anticoagulants (DOACs) have become the preferred anticoagulant medication for patients with nonvalvular atrial fibrillation, deep vein thrombosis, and pulmonary embolism. However, recent case reports show life threatening bleeding with DOAC use.
Apixaban is a direct factor Xa inhibitor that is used commonly to prevent stroke in nonvalvular atrial fibrillation and in the prevention and treatment of blood clots in pulmonary embolism and deep vein thrombosis. Direct factor Xa inhibitors are alternatives to the well-known warfarin and for some patients are preferred given convenient dosing, no laboratory monitoring, less interactions with other medications and reported decreased bleeding risk.1 Despite this reported decreased risk, bleeding remains a common adverse effect of apixaban with gastrointestinal and intracranial bleeding reported as most common.2-3
One rare bleeding complication is the development of spontaneous hemopericardium.4-7 There are a few case reports that document the development of this condition in patients on apixaban, with the first case series of this in the United States reported in 2015.3 We present a case of spontaneous hemopericardium in a patient on apixaban, specifically the development of spontaneous hemopericardium during sexual intercourse in an older gentleman in his seventies. There are no documented cases of the development of hemopericardium in association with exertional activity, in this case, sexual intercourse. We discuss sildenafil use as a potential serious drug-drug interaction with apixaban. We also discuss reperfusion injury as a potential mechanism for bleeding after coitus. This case highlights the importance of reiterating bleeding risks to patients on anticoagulation, especially the possible development of spontaneous hemopericardium during sexual activity.
CASE REPORT
A 75-year-old Caucasian male presented to the ED with the chief complaint of severe shortness of breath, acute distress, and hypotension. He had a past medical history significant for hypertension, hyperlipidemia, benign prostatic hyperplasia, B12 deficiency, obstructive sleep apnea, erectile dysfunction, and atrial fibrillation on chronic anticoagulation with apixaban 5 mg BID. He had been on apixaban for 11 months. His other medications included losartan, extended-release diltiazem, cyanocobalamin, furosemide, hydralazine, atorvastatin, finasteride, and sildenafil. He was not on any antiplatelet agents. The patient was having sexual intercourse with his wife when he developed sudden onset shortness of breath and suffered a near syncopal episode. The patient’s blood pressure on arrival was 53 mmHg/palp, heart rate of 83 beats per minute and saturating 100% on 2 liters of oxygen by nasal cannula.
Shortly after arrival, a chest x-ray (Figure 1) and a bedside echocardiogram were performed to evaluate the patient’s shortness of breath and hypotension.

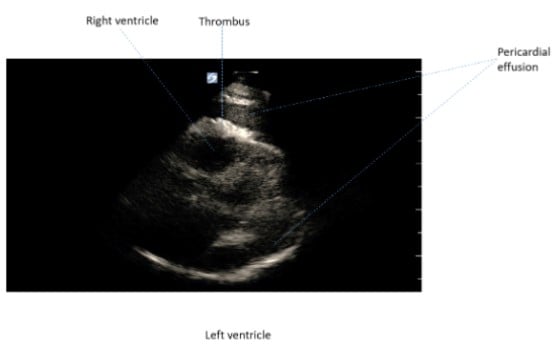
His chest x-ray revealed severe cardiomegaly and his echocardiogram demonstrated a large pericardial effusion with evidence of tamponade physiology. The patient was started on vasoactive medications with an initial increase in his blood pressure to 90mmHg systolic. However, after escalating doses of vasopressors and volume resuscitation the patient’s mentation worsened and he became more dyspneic and hypotensive. An attempt at bedside pericardiocentesis under ultrasound guidance was unsuccessful. The patient appeared to have developed a thrombus in the pericardial space, inhibiting successful drainage of the pericardial sac with a needle technique (figure 2).
Soon after the patient lost pulses. Cardiopulmonary resuscitation was started, the patient was intubated, and after verbal consent was obtained from the patient’s wife an emergent subxiphoid pericardiotomy was performed in the ED by the on-call cardiothoracic surgeon. Eight hundred (800) ccs of blood and clot were evacuated from the pericardial space and the patient immediately regained pulses. He was taken directly to the operating room where a median sternotomy was performed given concern for persistently active bleeding. The pericardium was marsupialized and additional blood clot evaluated. Complete exploration of the heart revealed no evidence of aortic or coronary dissection, no cardiac chamber bleeding, no epicardial inflammation, and normal pericardial thickness. A surface of epicardium near the coronary sinus was found to have muscle and epicardial bleeding without an involved vessel. This was repaired with pledgeted sutures and bioglue. Labs at the time of ED arrival showed no evidence of thrombocytopenia, uremia, coagulopathy, or anemia.
After being transferred to the intensive care unit he required up to 4 vasoactive medications and was transfused with multiple units of blood products, cryoprecipitate, factor 7 and 9, and activated prothrombin complex concentrate. It was understood that these interventions would likely not reverse the effects of apixaban. Andexanet alfa was not available for administration. The patient developed cardiogenic and hypovolemic shock, upper gastrointestinal hemorrhage, oliguria, severe acidosis, and right-sided hemiparesis. He ultimately died 24 hours after his initial presentation.
DISCUSSION
A multitude of research studies show DOACs are associated with lower risk of major bleeding when compared with warfarin. This has made DOACs a leading first-line medication for nonvalvular atrial fibrillation patients. However, recently there have been several case reports of DOACs such as direct factor Xa inhibitors and direct thrombin inhibitors causing spontaneous bleeds, including in the pericardium.4-7 Many of these case reports cite drug-interactions such as common CYP450 medication inhibitors,7 herbal products,5 and renal failure8 as likely causes. A medication review of our case reveals our patient was on 180 mg of extended-release diltiazem and 20 mg sildenafil, both notable CYP450 inhibitors. Additionally, a recent in vitro study shows sildenafil may significantly block apixaban and rivaroxaban cell efflux via p-glycoprotein inhibition, thereby increasing DOAC intestinal absorption and potentially increasing bioavailability and subsequent bleeding risk.8 Given these research studies, we postulate regular sildenafil use prior to sexual intercourse in patients taking DOACs may be a risk factor for spontaneous serious post-coital bleeding.
Currently, it is unclear whether exertional activity such as sexual intercourse is a risk factor for cardiac bleeding in patients on DOACs. We propose a theory where exertional activity such as coitus may cause myocardial ischemia in older vasculopathic patients, leading to subsequent reperfusion injury. During reperfusion injury, increased intracellular calcium, increased supply of oxygen free radicals, and subsequent inflammatory response may trigger bleeding in patients taking DOACs. However, recent studies have shown exercise as a potential protective factor via heat shock proteins, extracellular vesicles containing antioxidants, and improved mitochondrial function.9-12 In our patient it is unclear if the exertional activity itself played a role in his spontaneous muscle and epicardial bleeding. Our case could present a possible refutation of exercise as a potential protective factor in preventing reperfusion injury.
CONCLUSION
This case highlights the importance of reiterating the bleeding risks to all patients on anticoagulation. It is imperative to counsel patients, particularly older individuals, about the rare but possible development of spontaneous hemopericardium when engaging in sexual activity. Phosphodiesterase inhibitors such as sildenafil and other medications such as calcium channel blockers may decrease the metabolism of DOACs leading to increased bleeding risk. Exertional activity such as sexual intercourse, once thought to be protective against reperfusion injury, may lead to spontaneous bleeding. Although it is difficult to know to what extent these factors contributed to spontaneous hemopericardium, we highlight life threatening bleeding as a rare side effect in patients taking DOACs with sildenafil and diltiazem.
REFERENCES
- Bahit, M. C., Lopes, R. D., & Wojdyla, D. M. et al. (2017). Non-major bleeding with apixaban versus warfarin in patients with atrial fibrillation. Heart, 103, 623–628. Retrieved from https://heart.bmj.com/content/heartjnl/103/8/623.full.pdf
- Eisho, S., Salem, N. M., Hoffman, J. L., Koerber, J. M., & Smythe, M. A. (2018). Major Bleeding With Apixaban in Atrial Fibrillation: Patient Characteristics, Management, and Outcomes. Hospital Practice, 46(4), 165–169. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30058431/
- Sigawy C., Apter S., Vine J., Grossman E. Spontaneous hemopericardium in a patient receiving apixaban therapy: first case report. Pharmacotherapy. 2015;35:e115–e117.
- Asad ZUA, Ijaz SH, Chaudhary AMD, et. al. (2009). Hemorrhagic Cardiac Tamponade Associated with Apixaban: A Case Report and Systematic Review of Literature. Cardiovascular Revascularization Medicine, 20(11), 15–20. Retrieved from https://www.sciencedirect.com/science/article/pii/S1553838919302283
- Shivamurthy, P., Brar, N., & Therrien, M. L. (2014). Isolated Hemopericardium Associated With Rivaroxaban: First Case Report. Pharmacotherapy, 34(9),169–172. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25074401/
- Menendez, D., & Michel, J. (2016). Hemopericardium with tamponade following rivaroxaban administration and its attenuation by CYP3A4 inhibitors. Baylor University Medical Center Proceedings,4,414–415.Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5023303/
- Oladiran, O., Segal, J., Nwosu, I., & Nazir, S. (2016). A Rare Case of Spontaneous Cardiac Tamponade Induced by Concomitant Use of Rivaroxaban and Amiodarone. Case Reports Cardiology. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30159173/
- Margelidon-Cozzolino, V., Hodin, S., Jacqueroux, E., Delezay, O., Bertoletti, L., & Delavenne, X. (2015). In Vitro Assessment of Pharmacokinetic Drug-Drug Interactions of Direct Oral Anticoagulants: Type 5-Phosphodiesterase Inhibitors Are Inhibitors of Rivaroxaban and Apixaban Efflux by P-Glycoprotein. Journal of Pharmacology and Experimental Therapeutics, 365(5), 519–525. Retrieved from http://jpet.aspetjournals.org/content/365/3/519
- Kavazis, A. N. (2009). Exercise Preconditioning of the Myocardium. Sports Medicine, 39, 923–935. Retrieved from https://link.springer.com/article/10.2165/11317870-000000000-00000
- Levine, G. N., Steinke, E. E., & Bakaeen, F. G. (2012). Sexual Activity and Cardiovascular Disease. Circulation, 125(8), 1052–1072. Retrieved from https://www.ahajournals.org/doi/full/10.1161/CIR.0b013e3182447787
- Vishwakarma, V. K., Upadhyay, P. K., Gupta, J. K., & Yadav, H. N. (1995). Pathophysiologic role of ischemia reperfusion injury: A review. Journal of Indian College of Cardiology, 7(3), 97–104. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S1561881116301365.
- Apixaban: Drug information. (n.d.). Retrieved April 5, 2020, from https://www.uptodate.com/contents/apixaban-drug-information



