The best treatment for heat-related illnesses is public education and prevention. How can you help from your ED?
Heat-related illness is classically taught to represent a spectrum of hyperthermic disease ranging from heat cramps, heat syncope, heat exhaustion, and – in extreme cases – heat stroke. Symptoms present when the body is exposed to heat with inability to properly cool core body temperature. Normal core temperature ranges between 36-38° Celsius. Below 35° C, radiation represents 60% of heat dissipation with an additional 30% from evaporation; above 35° C, this native process becomes overwhelmed and insufficient to maintain adequately cooled core body temperature. Subsequently, thermoregulatory failure occurs and the body is unable to release heat quickly, leading to elevated core temperatures.
Incidence and Risk Factors
Between 1999 and 2010, 8081 heat-related deaths were reported in the United States, with 94% of deaths occurring between May in September.1 Because reporting of heat-related illness is not mandatory, the incidence is likely underestimated. A heat wave is defined as >3 consecutive days of sustained temperatures > 32.2° C or 90°Fahrenheit.
Non-environmental risk factors include heavy clothing or equipment, children younger than 4 years of age, adults older than age 65, obesity, and underlying medical conditions such as diabetes, heart, and pulmonary disease. Young individuals participating in strenuous activity during warm weather increases their risk of heat-related illness. Environmental risk factors include warm temperatures and humidity, especially in populations not acclimated to them, and can be exacerbated by lack of access to transportation, medical care, and cooling centers.
Types of Heat Illness
Heat-related illness may be classified as exertional or non-exertional (classic). Exertional type is related to the endogenous heat production of physical activity and generally occurs in young, healthy individuals. Non-exertional type tends to be environmentally related and occurs insidiously in children and the elderly.
Classic heat-related illness occurs during periods of high environmental heat stress, and physical exertion is not required. In non-exertional heat illness, the increase in core temperature is generally slow, occurring over hours to days. Subsequently, these individuals are likely to develop volume or electrolyte disturbances.
Exertional heat injuries tend to occur in young, physically fit individuals performing under conditions of high heat, including sports, recreational physical activity, firefighting, and military training.
Treatment
The best treatment for heat-related illnesses is public education and prevention. Air-conditioning is the No. 1 protective factor against developing heat-related illness and death.2 During a heat wave, public facilities with air conditioning should be made available.
In mass participation events, several measures can be taken by organizers and medical staff to reduce the risk of developing heat-related illness. Care should be taken to avoid scheduling during hot and humid months, and events should be held during the cooler hours of the day. If possible, athletes should prepare with heat acclimatization; a process of increasing activity duration and intensity during the preceding 10-14 days.
Athletes should have fluid intake, diet, and whole-body sodium levels monitored, wear lightweight, light-colored and loose-fitting clothing, and have shaded areas available for rest and recovery.
Finally, coaches, athletes, administrators, and medical providers should be educated on prevention, recognition, and treatment of heat-related illness.
Heat edema is a self-limited process defined as dependent pretibial edema of the lower extremities and/or hands during the first few days of exposure to increased temperature. Although it usually resolves within days of onset, patients may be symptomatic for up to 6 weeks. No specific treatment is necessary; elevation and compression stockings may accelerate recovery and aid in symptomatic relief. Diuretics are not indicated and may precipitate more severe heat-related illness.
Prickly heat, also known as miliaria rubra or heat rash, is a pruritic, maculopapular, erythematous rash due to inflammation, dilation, and rupture of the sweat glands, producing small vesicles that presents over clothed areas of the body. Patients generally complain of itching, which responds well to antihistamines. Wearing light, loose-fitting clothing will reduce likelihood of developing heat rash. Talc and baby powder do not help; chlorhexidine lotion may provide relief.
Heat cramps are painful, involuntary muscle contractions, typically of the calves, occurring in sweating individuals with inadequate volume replacement or who are hydrating with hypotonic fluids. Cramps may occur during exercise or commonly during a rest period following physical activity. Although self-limited, patients may present to the emergency department due to persistent myalgias. Cramping is usually isolated to a specific muscle group and rarely leads to the development of rhabdomyolysis.
Electrolyte disturbances include hyponatremia and hypochloremia. Primary treatment is with oral isotonic fluid replacement and rest in a cool environment. Oral hydration with 0.1% saline solution or with commercially available electrolyte drinks are adequate for most patients. Patients with severe symptoms may require IV rehydration. Prevention is directed at maintaining sufficient hydration with either water and salt tablets or commercial electrolyte drink.
Heat tetany is caused by hyperventilation and subsequent respiratory alkalosis, presenting as paresthesias of the extremities, perioral area, and carpopedal spasm. It is often confused with heat cramps; however, it is a separate clinical entity typically not accompanied by muscle cramps. Treatment is directed at moving the patient to a cooler area and reducing their respiratory rate.
Heat syncope is due to a combination of volume depletion, peripheral vasodilation, and decreased vasomotor tone resulting in postural hypotension. Evaluation includes workup of other causes of syncope including cardiac, metabolic, and neurologic etiologies, and treatment is directed at rehydration, rest, and removing the patient from the area of heat exposure. Hospitalization is often unnecessary.
Heat exhaustion is the result of both hypovolemia and hyponatremia. Hypovolemia occurs in individuals in warm environments with inadequate water replacement; hyponatremia occurs when individuals replace fluid losses with water or other hypotonic fluids. Symptoms include headache, nausea and vomiting, malaise, dizziness, muscle cramps, and other clinical indicators of hypovolemia. Notably, patients do not have altered mentation. Patients are tachycardic and may have positional hypotension, temperature is elevated
but typically below 40° C. Laboratory evaluation reflects hemoconcentration; patients may have hypotonic or isotonic hypovolemia. Treatment is directed at fluid replacement, electrolyte correction, removal from warm environment and rest. These patients may require active cooling, especially if not responding to the first 30-60 minutes of therapy.
Traditionally heat-related illness has been presented as a spectrum of hyperthermic disease; however, there is a lack of consensus in the literature that heat cramps, heat syncope, and heat exhaustion progress to or increase the risk of heat stroke. While many of these previously described phenomena can occur in the presence of increased temperatures, they can also occur in its absence. Alternative pathophysiologic mechanisms independent of heat have been proposed; such as neuromuscular control theory for exercise induced muscle cramps8 or heat syncope explained as exercise associated collapse in the presence of heat by the Edholm-Barcroft reflex as described by Noakes.9
While investigation into the pathophysiology of these disease states continues, the risk of referring to them as a spectrum of hyperthermic illness may overstate their clinical significance as it relates to the most important diagnosis caused by increased temperature: heat stroke.
True Medical Emergency
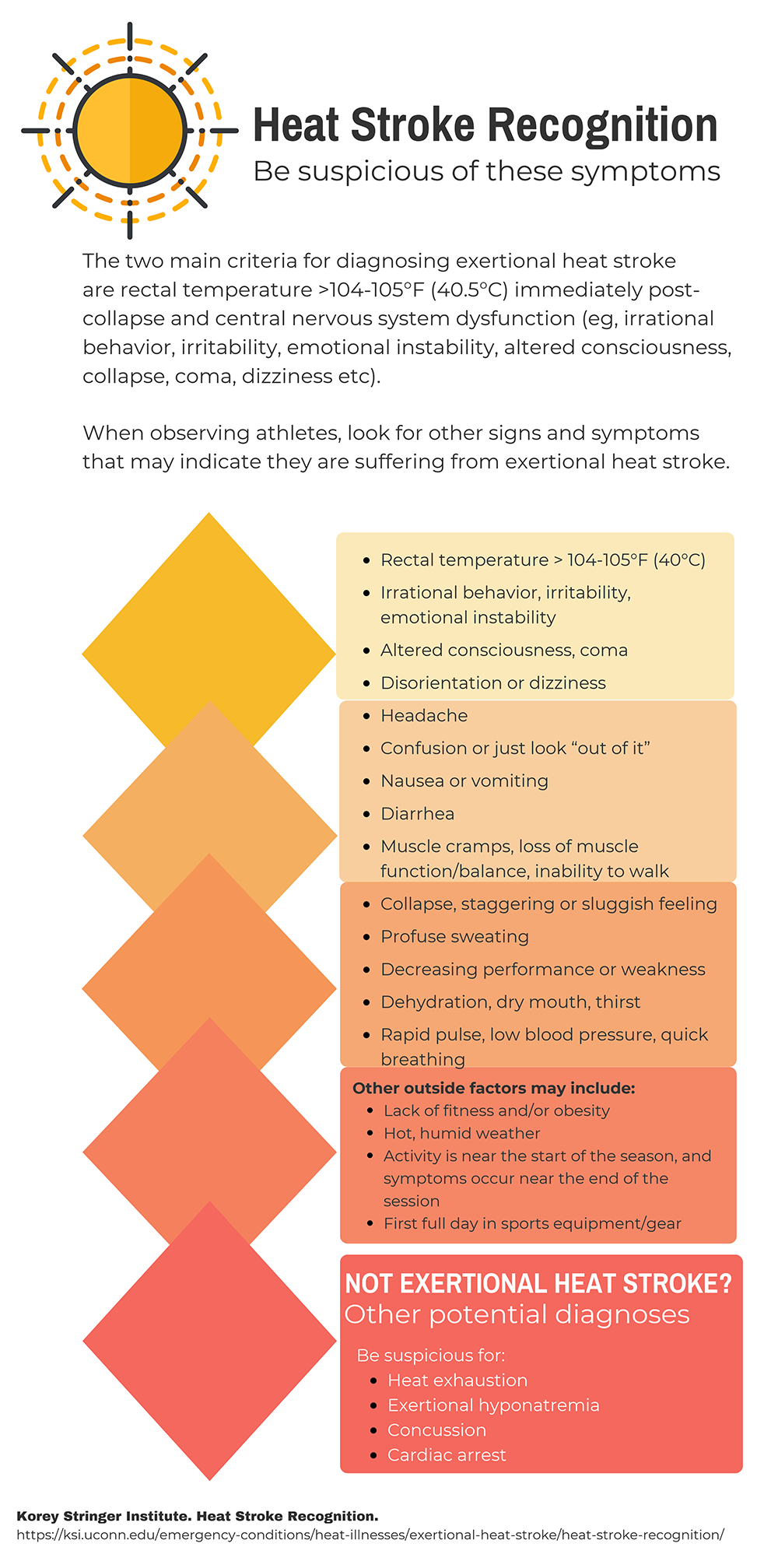
Heat stroke, whether classical or exertional, is the most serious presentation of heat-related illness. Mortality rates range from 30-80% and is universally fatal if left untreated. The diagnosis is generally clinical and defined by encephalopathy and hyperthermia > 40° C, although temperature less than 40° C should not be exclusive criteria for treatment.
The presence of mental status changes in a hot and/or humid environment should be considered heat stroke until proven otherwise. Anhidrosis is not diagnostically reliable. Ataxia is an early symptom due to sensitivity of the cerebellum; patients may also have irritability, confusion, behavior changes, combativeness, hallucinations, decorticate and decerebrate posturing, hemiplegia, and coma. Seizures are common. Neurologic injury is a function of duration of exposure and maximum temperature. The patient may be tachycardic, tachypneic, and/or hypotensive.
Heat Stroke Management
Initial treatment of exertional heat stroke is directed at removing the patient from the offending environment and immediate cooling with cold-water immersion, as it has been shown to be the fastest cooling modality.7 If cold water immersion is not available, cold water dousing and wet ice towel rotation may be used, but these have not been found to be as efficient.
The length of time that core body temperature is elevated has been linked with increased morbidity and mortality, with practitioners aiming to lower body temperature below 39° C within 30 minutes to decrease these risks.5 Because external thermometry is unreliable, accurate temperature measurement with a core temperature is essential; regardless, cold-water immersion should be initiated as soon as the diagnosis is suspected.4 Rapid cooling should be discontinued once temperature reaches 39° C to avoid rebound hypothermia. Heat stroke is a medical emergency and patient should be transported to hospital for further evaluation.
In the ED, treatment is directed at addressing the ABCs of airway, breathing, and circulation, along with volume resuscitation and continued active cooling of the patient. Cold water immersion of body up to torso or diffuse application of ice and cold packs provide the most rapid decrease in temperature and the lowest morbidity and mortality. The disadvantage of these methods is it is more difficult to provide other resuscitative measures.
The United States military has developed an Arm Immersion Cooling System (AICS), which involves submerging one of the patient’s arms in ice water and may be as effective as full body immersion.6 Spraying cool water on patients with a fan directed at them is easy to initiate in the emergency department but provides slower cooling than immersion techniques. There is inadequate data to recommend invasive cold water lavage or ECMO. Antipyretics and dantrolene are not indicated for temperature reduction. Intravenous fluid resuscitation should be isotonic fluids with a target urine output of 2-3 mL/kg/hr.
It is important for the provider to consider other causes of altered mentation and to assess for end organ damage. Diagnostic studies include complete blood count, metabolic panel, blood gas, creatine phosphokinase, myoglobin, coagulation panel, urinalysis. An electrocardiogram and chest radiograph should be obtained. Lumbar puncture and head CT should be considered.
In the first 24-72 hours following heat stroke, organ system damage becomes evident, including ARDS, metabolic acidosis, respiratory alkalosis, electrolyte imbalance, hypoglycemia, increased CPK, rhabdomyolysis, leukocytosis, coagulation disorder, and hepatic dysfunction. Late complications include acute renal failure, pulmonary edema, stroke and hepatic failure. All patients presenting with heat stroke require admission to the hospital.
Return to Play
Individuals who experience exertional heat stroke should consult their physician prior to return to physical activity, as heat stroke itself can be a risk factor for repeat incidence. The 2007 American College of Sports Medicine guidelines suggest that those who suffered exertional heat stroke should be held from exercise for at least 7 days with follow up laboratory testing prior to return to any physical exertion.3
When cleared, a progression from exercise in cool environments indoors can be initiated with gradual increase in duration, intensity, and heat exposure if patients remain asymptomatic.
A progressive heat tolerance test is frequently employed prior to granting clearance for return to full activity if a patient experiences difficulty with the ACSM guidelines.
References
1. Centers for Disease Control and Prevention. Picture of America Report: Heat-Related Illness. Accessed July 2018.
2. Davis RE, Knappenberger PC, Novicoff WM, Michaels PJ. Decadal changes in heat-related human mortality in the eastern United States. Climate Research. 2002;22(2):175–184.
3. Armstrong LE, Casa DJ, Millard-Stafford M, et al. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39:556-572.
4. Casa DJ, Becker SM, Ganio MS, et al. Validity of Devices That Assess Body Temperature During Outdoor Exercise in the Heat. J Athl Train. 2007;42(3):333-342.
5. Costrini A. Emergency treatment of exertional heatstroke and comparison of whole body cooling techniques. Med Sci Sports Exerc. 1990;22(1):15–18.
6. DeGroot DW, Gallimore RP, Thompson SM, Kenefick RW. Extremity cooling for heat stress mitigation in military and occupational settings. J Thermal Biol. 2012;38(6):305-310.
7. Hadad E, Rav-Acha M, Heled Y, Epstein Y, Moran DS. Heat Stroke: a review of cooling methods. Sports Med. 2004;34(8): 501-511.
8. Schwellnus MP, Derman EW, Noakes TD. Aetiology of skeletal muscle ‘cramps’ during exercise: A novel hypothesis. J Sports Sci. 1997;15(3):277-285.
9. Noakes TD. A modern classification of the exercise-related heat illnesses. J Sci Med Sport. 2008;11(1):33-39.
10. Korey Stringer Institute. Heat Stroke Recognition. Accessed September 2018.