Freestanding emergency departments offer risks and rewards to our health care system.
In the 1970s, the freestanding emergency department (FSED) emerged in rural areas to provide access to emergency care for residents living without a nearby acute care hospital. FSEDs offer emergency medical care at locations independent from hospitals. Growth in the number of FSEDs and the services rendered by these facilities varies widely from state to state, largely mirroring the regulatory structure in those locales.
This study identified 21 states that had regulations allowing FSEDs and twenty-nine states that had no specific policy toward these facilities. Of the states with policies specific to FSEDs, the study found significantly differing policies pertaining to permitted geographic locations for the facilities, required services, mandated equipment, staffing requirements, hospital affiliation, and whether a certificate of need was necessary for the creation of the facility. Unsurprisingly, states with stringent requirements regarding the creation, staffing, and activities of FSEDs saw dramatically less growth of these facilities. California, for instance, requires that surgical services be available immediately at all FSEDs. Alabama requires a certificate of need from the state to establish a FSED and requires all FSEDs to have a helipad. The statutes in these states are strict enough to largely or completely prohibit the creation of FSEDs.
Given the recent national trend of rural hospital closure, FSEDs remain a viable method of providing access to care in medically underserved areas. Further, FSEDs could also play an important role in reducing ED overcrowding in urban areas.
Conversely, increased availability of FSEDs could increase utilization of emergency care in circumstances that are nonemergent, increase health care costs, and siphon insured patients away from larger hospital systems who largely bear the financial burden of caring for the uninsured.
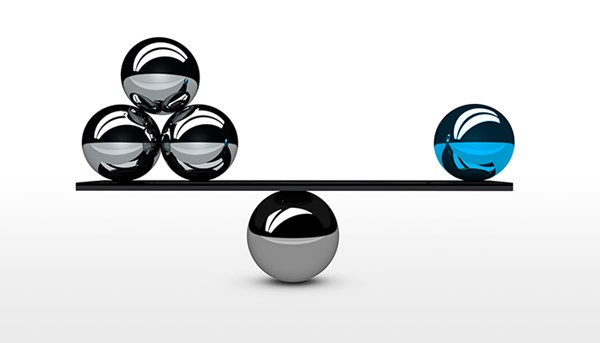
Moving forward, it would be prudent of policy makers to structure FSED regulatory policy to appropriately strike a balance between access to care and fiscally sustainable health care cost growth. For example, a state may implement statutes that curb the growth of emergency care facilities based on the per capita availability of emergency department beds. A rule of this nature would allow for free market innovation to accommodate demand while inhibiting over-expansion and the associated danger of increased health care costs.
ARTICLE: Gutierrez C, Lindor RA, Baker O, Cutler D, Schuur JD. State Regulation of Freestanding Emergency Departments Varies Widely, Affecting Location, Growth, and Services Provided. Health Aff (Millwood). 2016;35(10):1857-1866.
ABSTRACT: Freestanding emergency departments (EDs), which offer emergency medical care at sites separate from hospitals, are a rapidly growing alternative to traditional hospital-based EDs. We evaluated state regulations of freestanding EDs and describe their effect on the EDs' location, staffing, and services. As of December 2015, 32 states collectively had 400 freestanding EDs. Twenty-one states had regulations that allowed freestanding EDs, and 29 states did not have regulations that applied specifically to such EDs (one state had hospital regulations that precluded them). State policies regarding freestanding EDs varied widely, with no standard requirements for location, staffing patterns, or clinical capabilities. States requiring freestanding EDs to have a certificate of need had fewer of such EDs per capita than states without such a requirement.
CONCLUSIONS: For patients to better understand the capabilities and costs of freestanding EDs and to be able to choose the most appropriate site of emergency care, consistent state regulation of freestanding EDs is needed. PMID: 27702960
EMRA + PolicyRx Health Policy Journal Club: A collaboration between Policy Prescriptions and EMRA
 As emergency physicians, we care for all members of society, and as such have a unique vantage point on the state of health care. What we find frustrating in our EDs - such as inadequate social services, the dearth of primary care providers, and the lack of mental health services - are universal problems.
As emergency physicians, we care for all members of society, and as such have a unique vantage point on the state of health care. What we find frustrating in our EDs - such as inadequate social services, the dearth of primary care providers, and the lack of mental health services - are universal problems.
As EM residents and fellows, we learn the management of myocardial infarctions and traumas, and how to intubate, but we are not taught how health policy affects all aspects of our experience in the ED. Furthermore, given our unique position in the health care system, we have an incredible opportunity to advocate for our patients, for society, and for physicians. Yet, with so many competing interests vying for our conference education time, advocacy is often not included in the curricula.
This is the gap this initiative aims to fill. Each month, you will see a review of a new health policy article and how it is applicable to emergency physicians.