Over the past 30 years, emergency care (EC) has rapidly developed in many places around the globe.1
As of May 2019, 82 countries recognize emergency medicine as a distinct specialty, and there are more than 80 EC-related journals worldwide.2,3 This growth stemmed from the recognition that conditions amenable to EC, such as trauma, cardiovascular disease, and strokes, are substantial contributors to global mortality (50.7%), as well as an increased understanding of EC’s capacity to reduce overall morbidity and mortality and promote the delivery of safe, efficient, and effective care.4,5 The World Health Organization spurred EC development through calls for comprehensive emergency health care systems that seamlessly integrate prehospital care with stabilization, triage, immediate care, and in-hospital care.6
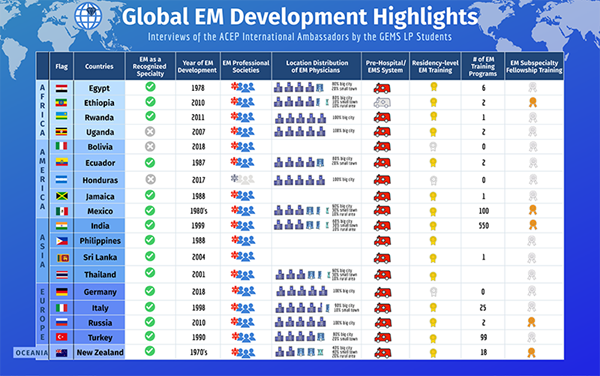
However, advancing EC is a tall task, often complicated by social, political, and economic factors. Therefore, emergency physicians eager to educate, research, and develop EC globally in conjunction with local partners are needed. ACEP’s International Ambassador Program seeks to do just that through collaborative efforts of teams consisting of U.S. and internationally-based emergency physicians. Currently, Ambassador teams are engaged in the development of EC in 79 countries. Medical students from the Global Emergency Medicine Student Leadership Program sat down with 18 of ACEP’s International Ambassador teams to capture their perspectives on the state of EC development in the countries where they work.
AFRICA
Egypt
Student Interviewer: Rebecca Leff
Ambassador Team Interviewee(s): Dr. Jon M. Hirshon (ACEP Lead Ambassador), Dr. Walid Hammad (ACEP Deputy Ambassador)
“[When considering emergency medicine capacity building in the setting of a LMIC like Egypt] don’t go for the bells and whistles and all the newest gadgets, go for what is most important from a population-based perspective... Our global partners know what they need. Our job as global health practitioners is to support them.”
Exciting Development
The most encouraging advancements are the development of the specialty and solidification of the foundational proficiencies of EM. For example, the success of the Sequential Trauma Emergency/Education Programs course, created through a collaborative effort of the University of Maryland and Egyptian physicians, has been demonstrated by over 1000 physicians being trained in trauma care and by the program’s perpetuation after transitioning to in-country trainers and direction.
Biggest Challenge
While the number of physicians trained in EM has significantly increased over the past decade, "brain drain" has taken a significant toll on the expansion of EM in the country, as newly trained EM physicians emigrate to practice in other, more lucrative settings.
Ethiopia
Student Interviewer: Rio Beardsley
Ambassador Team Interviewee(s): Dr. Getaw Hassen (ACEP Lead Ambassador)
“It’s all about the lack of resources – we’re developing the international [academic] connections, we have the students, but it’s all limited because it’s hard to even get a CT scan in most places.”
Biggest Challenge
Resource shortages, specifically the lack of medication and equipment are two of the biggest barriers to improving emergency care in the country.
Ambassador Team’s Work
A current research project is investigating the use of ultrasound to measure optic sheath diameter as a surrogate measure for outcome severity in traumatic brain injuries.
Rwanda
Student Interviewer: Natalie Jansen
Ambassador Team Interviewee(s): Dr. Adam Levine (ACEP Lead Ambassador)
“In the U.S. sometimes we don’t have access to a medication or a tool that we’re used to using - and we sort of shut down. One thing you learn in resource-limited settings is that you can continue practicing. You can continue working. No matter what is gone you can just figure out a way to do whatever you can that’s best with the resources you have.”
Exciting Development
There are now fully trained Rwandan EM faculty who are running the EM training program and the ED. Additionally, a government policy change to waive a two-year service requirement if pursuing EM has helped facilitate additional interest and demonstrates that EM is a priority.
Biggest Challenge
The biggest challenge is access to resources, both financial and human. Investment in medical trainees takes years and once they’ve been trained there is the additional challenge of finding money to pay their salaries and keep them in the country. “There are going to be limitations in supplies, equipment, and facilities...but, I think the limitations of human resources are by far the most important because you can have a fancy new EKG machine, but if no one knows how to read an EKG, it's not going to be very useful.”
Uganda
Student Interviewer: Kelley Gorsuch
Ambassador Team Interviewee(s): Dr. Stacey Chamberlain (ACEP Lead Ambassador)
“I tend to focus in my clinical practice on clinical reasoning… and minimizing clinical tests. Working and observing in an environment where there [are] extremely limited diagnostic tests… you see where there can be a balance”.
Exciting Development
Mbarara University of Science and Technology is celebrating the recent graduation of their first class of EM residents from its two-year master’s program. The inaugural class of five graduates comes at a crucial time during the growth of emergency care in the country.
Biggest Challenge
"...It is exciting that 5 or 6 people have just graduated... it is still not going to be enough for the whole country." The biggest challenge remains the access to care in rural areas. "...There will still be a large gap in care for rural areas (~80% of the population) even with this exciting advancement."
AMERICAS
Bolivia
Student Interviewer: Ricki Sheldon
Ambassador Team Interviewee(s): Dr. Autumn Brogan (ACEP Lead Ambassador), Dr. Ashley Jacobsen (ACEP Resident Representative)
Exciting Development
The first International Congress for Emergency, Trauma and Disaster Medicine (Primer Congreso Internacional de Medicine de Emergencias Trauma y Desastre) was planned for March 2020 but was postponed due to COVID. These well-publicized meetings with the involvement of international EM organizations and physicians will help promote EM for national recognition as a specialty.
Biggest Challenge
Hospital systems need to publish research in the field of EM in order to gain credibility for the specialty. Once an institution produces a number of publications, the government can consider its ability to create an EM residency.
Ecuador
Student Interviewer: Halley Alberts
Ambassador Team Interviewee(s): Dr. Agusto Maldonado (ACEP Liaison)
"Just like all the countries in the world, the role of the initial responders and the organization of emergency services in the face of this health emergency [COVID-19] has been very special. I believe that to the authorities, it is now very clear the importance of emergency medicine as a specialty to face this type of complex situation”
Exciting Development
Sociedad Ecuatoriana de Medicina de Emergencias, has increased in number by over 500%! The society has been very active at the national level to define treatment protocols for COVID patients and establish national policies. The society has also shown initiative in exploring specific areas of EM, such as pediatric emergency care.
Biggest Challenge
There are large disparities, between private and public healthcare sectors and between rural and urban areas such as shortages in medical supplies, long wait-times, and crowding. Additionally, the economic situation has limited innovation. Many EM providers are having to work two to three jobs to have a sufficient income to live, leaving little time for research, teaching, or collaboration.
Honduras
Student Interviewer: Francesca Brancati
Ambassador Team Interviewee(s): Dr. Rosa Tercero (ACEP Liaison)
Exciting Development
The National Emergency System (SNE) was established in 2017. This law created a ‘911’ phone number for any type of emergency and instituted ambulances to provide pre-hospital care and inter-facility transport. Prior to this, citizens had to be brought to the nearest hospital by family members, cab, or police car. There are now 52 ambulances in Honduras located in seven major cities. These ambulances are staffed by first responders who undergo a year of medical training, including basic life support, and are the equivalent of an EMT-intermediate.
Biggest Challenge
Developing a “consciousness in the medical community” for the specialty of EM has been a challenge. EDs in Honduras are currently operated by general practitioners or specialists, with no real triage system in place. Creating an EM specialty would require integrating EM physicians with the current structure and “introducing the philosophy of EM” to medical practice, which requires gaining the support of hospital systems and physicians.
Jamaica
Student Interviewer: Ololade Akinfemiwa
Ambassador Team Interviewee(s): Dr. Vanessa Cousins (ACEP Deputy Ambassador)
"[You learn] how to make do with what you have. How to best utilize your resources. I remember once I was trying to get an ultrasound. I was so used to being able to get an ultrasound and putting an IV in. I had to use a transvaginal probe at one point, to put in an IV, which was interesting…”
Biggest Challenge
The greatest challenge is limited resources and staff. “It is a mix between physicians and nurses. They have good nursing staff, but they are still really limited. More so the resources, though. The facility, the equipment, and the medicine themselves.”
The Ambassador Team’s Work
One goal is to “develop some resources, such as handouts that we can send that they can give to their residents. For example, a quick handout about something pharmaceutical that is helpful clinically.” Another “is to figure out how to get ACLS done with limited funding and resources. It is a little more challenging, but I think once we can get some things virtually set up, I think that will be a great way to help in terms of developing those handouts or whatever it is that we use for education.”
Mexico
Student Interviewer: Nathan Bode
Ambassador Team Interviewee(s): Dr. Haywood Hall (ACEP Lead Ambassador), Dr. Jorge Garcia (ACEP Liaison)
“[International collaboration] is the best opportunity to improve our practice. It makes us improve our curriculum, our programs, and our training. [However, local participation in conjunction with international work is important] to show that they are doing something in their own country at some level, and to make sure that the needs of local organizations are also being prioritized.”
Exciting Development
Over 30 residency programs opened in the last two years. This is a significant achievement as there are now at least two EM residency programs in each of the 31 Mexican states with almost 400 new practitioners completing residency each year. Dr. Hall speculates that Mexico is on track to become one of the top 5 countries in the number of EM-trained physicians. “I think Mexico is a model for the development of EM, and I’m glad they’re finally getting the spotlight.”
Biggest Challenge
Along with the significant growth of EM comes growing pains. Mexican EM physicians “are the new kids on the block” and must now find their position in the pecking order among other specialties with longer, more integrated histories in Mexican medicine.
EUROPE
Germany
Student Interviewer: Tammy Tarhini
Ambassador Team Interviewee(s): Dr. Thomas Fleischmann (ACEP Liaison)
“Never accept no as an answer [when pushing for EM development].”
Exciting Development
Though not yet recognized as a specialty, the development of hospital-based emergency care has finally begun to find footing. This development follows a 2018 piece of legislation from the German Medical Council describing minimum standards for hospital emergency care, to be implemented by state medical councils over a 5-year transition period. This led to the creation of subspecialties in acute care and EM comprising two years of ED training following the completion of residency in another specialty.
Biggest Challenge
Emergency care in hospitals has historically been provided by many departments independent of each other, with each wanting to assume responsibility for their respective emergencies; chest pain to the cardiologists, abdominal pain to the internists, and so on. However, these departments often send junior doctors to receive these emergencies, “sometimes within months of graduating medical school”, contributing in part to over-testing and over-admission into already limited hospital beds.
Italy
Student Interviewer: Vian Zada
Ambassador Team Interviewee(s): Dr. Alexandra Asrow (ACEP Lead Ambassador)
"Patients are patients no matter where you go. Patients come with the same stuff, in different languages. Whatever the difference is, it's in the systems and treating the patients is the same. You can take what you learn anywhere.”
Exciting Development
7 to 10 years ago, there were 500-600 EM residents in the country. For comparison, 800 people applied this year alone. This spike in interest and enthusiasm for the EM field - which was previously struggling for recognition - started just before COVID-19.
Biggest Challenge
The Italian Society of Emergency Medicine continues to seek ownership of EM’s unique skill set and legitimacy from other specialties such as some anesthesiology societies, who have control over critical care and many procedures like central lines and intubations.
Additionally, the quality of prehospital care varies widely between regions and tends to be localized to major cities. A large number of ambulance staff are volunteers; with requirements to work on an ambulance dependent on the region, and there are no national prehospital care guidelines or standard operating procedures. Transfer to higher specialty care is thus more feasibly achieved in the north, where hospitals are larger and less crowded, and physicians tend to be better prepared. South of Naples, mortality and morbidity rates are higher due to this disparity in prehospital and hospital access.
Russia
Student Interviewer: Sean Flannigan
Ambassador Team Interviewee(s): Dr. Anthony Rodigin (ACEP Lead Ambassador)
“Most physicians go into medicine for the right reasons and are not motivated monetarily. However, those choosing "emergency care" still face largely pre-hospital work due to a low number of functional EDs.”
Exciting Development
“Emergency care” as a specialty now recognized by law to include an in-hospital component. Over twenty EDs have opened up in various regions, though restricted to major cities. A national EM society is fairly active, pushing for further reforms.
Biggest Challenge
Tightening of the regime’s budget as the ruble drops comparatively to the USD and Euro has translated into fewer resources for EM in the country. This has resulted into an effective stagnation of progress in EM. Leaders in the field stationed mainly in St. Petersburg push to maintain past accomplishments as the government shifts its focus towards politics and civil unrest.
Turkey
Student Interviewer: Wesley Steeb
Ambassador Team Interviewee(s): Dr. Cem Oktay (ACEP Liaison), Dr. Sabak Mustafa (ACEP Liaison)
"Emergency care in Turkey continues to expand after its initiation as a residency-trained specialty in 1993 making it one of the oldest emergency medicine residencies in Europe"
Exciting Development
Along with the expansion of residency training, the physical size of EDs has expanded in recognition of the importance of emergency care in achieving public health goals and patient safety. The expansion has also included equipment, especially ultrasound.
Biggest Challenge
With such rapid growth, identifying and retaining faculty remains the greatest challenge to fostering the continued growth of EM as a specialty. There are only 300-350 emergency medicine faculty in the country. We don’t have enough attending physicians specifically for training hospitals. … It’s a big problem for the residents, they don’t get enough education specifically on the night shifts.”
ASIA, OCEANIA, AND THE PACIFIC
India
Student Interviewer: Jemima Stanley
Ambassador Team Interviewee(s): Dr. Lingappa S. Amermath (ACEP Lead Ambassador)
"You are not going to be ordering all sorts of tests, imaging, CAT scans, MRI on a person who makes $100 a month and wipeout his income looking for zebras. It’s very focused (and involves) very limited tests. If you are in a corporate hospital, you are going to be doing similar tests to what we do (in the US). Cost is not a factor for them, and patients want everything done because they are happy to pay for it. It’s a different practice, so I would say modify it according to where you are. If you are in Rome, be a Roman.”
Exciting Development
EM was recognized as a new academic discipline in 2009. Even after this occurred, there was still a lot of debate on the implementation of EM training due to the lack of resources (such as faculty) and buy-in from the people. However, in October 2020 a law was passed by the Indian government to mandate that medical schools have an ED in their teaching hospitals and a Medical Council of India approved a 3-year EM residency program. This was a huge milestone in the development of EM in India.
Biggest Challenge
There are 1500 EM physicians for 1.3 billion people. To put this into perspective, the overall density of EM physicians per 100,000 population is 0.115 in India as compared to 14.9 in the USA.
New Zealand
Student Interviewer: Grace Brown
Ambassador Team Interviewee(s): Dr. Michael Connelly (ACEP Deputy Ambassador)
“It’s always our goal to provide the best care, but we are trying to be more outspoken about how we deliver that...and set up that feeling of cultural safety within EDs in New Zealand.”
Exciting Development
Australian College for Emergency Medicine has committed to equity for Māori through the launch of a strategy called Manaaki Mana: Excellence in Emergency Care for Māori, in 2019. It seeks to tackle the challenges of health equity, especially in the ED. Although some gains have been made over the past 30 years to improve health outcomes for Māori, there continue to be consistent and large disparities in health outcomes, exposure to the causes of poor health, inadequate health system responsiveness, and under-representation of Māori in the health workforce.
Biggest Challenge
One of the biggest strains on the ED, is access block and the use of the ED as a type of short-stay ward. The Ministry of Health is recognizing the importance of the efficient disposition of patients and has a target to move 95% of patients through the ED within six hours. “There isn’t enough space to see the patients coming in, and there isn’t enough movement in the hospital upstairs to move patients forward. So, it has really been a struggle to get hospitals to understand what happens upstairs affects the front door (the ED).” Currently, no District Health Board is meeting these targets, so there is still significant work to be done in this realm.
Philippines
Student Interviewer: Ogechi Nwodim
Ambassador Team Interviewee(s): Dr. Tao Zhu (ACEP Deputy Ambassador), Dr. Ted Herbosa (ACEP Liaison), Dr. Elis Maghirang (ACEP Liaison)
“We were seen as jack of all trades and master of none. But now, we as a specialty have been able to prove ourselves, not only in the emergency room but in other positions. Now, our colleagues have realized we are very good partners to work with, not only in the hospital but also elsewhere.”
Exciting Development
The most exciting development is the gain of respect for the specialty as a whole. Growth is exciting! Now the younger EM doctors are in disaster medicine, pandemic medicine, legislation, global health, and many other sectors in medicine. This growth was exemplified by the growth of the yearly EM society conference as well as increases in residency programs, public hospital EDs, and increased income for EM physicians.
Biggest Challenge
The greatest challenge is that the current supply of EM physicians is not meeting demand. “Many go to Australia to work with maritime cruise ships and oil rigs, or to be resort physicians in the Bahamas. This is good because the training is being recognized internationally, but they are leaving. Half of them want to leave and half of them will be gone in two years. It’s this double-edged sword, you see. We are proud that they are competent to work internationally, but we are also sad because the Philippines also needs more physicians nationally. This is the price that we have for our success.”
Sri Lanka
Student Interviewer: Shruti Gujaran
Ambassador Team Interviewee(s): Dr. Arun Nandi (ACEP Lead Ambassador)
"Half the time, the solution [is to] listen to the family, as they know the patient far better than you can. In a region where the income of a family can depend on one person, the existence of a family can depend on the health of one person. By listening to the family, to the patient, and even stuff that doesn’t make sense to you, it can be extremely valuable to you and to the longevity of the patient and community. "
Exciting Development
A virtual EM residency training effort has been organized over the past few years by several consultants from the US, UK, Singapore, and Australia to address the resource limitations for training residents. With the first EM consultants gradually starting in Sri Lanka, they will assume the crucial role of educating and training future generations of emergency physicians in Sri Lanka.
Biggest Challenge
Residents must go abroad to complete their training in their final year, which results in trainees who are exposed to technology and environments that they may not have access to at home. For example, “in their last year of training in the UK or Australia, learning point-of-care ultrasound, airway management… [residents] are learning in a country where you do things totally differently, resulting in an artificial learning curve.” To address this, infrastructure must be built within Sri Lanka, so residents are able to train locally within the tools available.
Thailand
Student Interviewer: Spencer Seballos
Ambassador Team Interviewee(s): Dr. Pholaphat Charlie Inboriboon (ACEP Lead Ambassador), Dr. Wirachin Hoonpongsimanont (ACEP Deputy Ambassador), Dr. Khuansiri Narajeenron
“[My global work] has given me a shift in mindset – thinking about resiliency; international physicians have a lot of barriers, like resource limitations and volume of patients. It reminds you that it’s also occurring elsewhere too – we’re all in this together. There are different systems in different countries, such as Thailand. They make you think about ways to make the system more efficient here: do we need to do all of these steps [in America]?”
Exciting Development
Recently, the Chulalongkorn University EM residency program developed the “Thai College of Emergency Physicians Application,” a tool to assist all residency programs in collecting trainees’ education portfolios and assessing their progress during residency training. This tool allows for the collection of country-wide data and comparison of trainee milestones (entrustable professional actions, procedure logs, conference attendance, and multisource feedback/evaluation tools) between programs. This application reduces the administrative burden of data collection and provides a dashboard to review results and share feedback.
Biggest Challenge
Thailand has fewer emergency physicians than other specialties. Additionally, the system does not encourage physicians to practice EM and serve as educators in the university setting. A significant challenge is the lack of an appropriate EM-specific reimbursement system that leads to low revenue in the department. The base salary for academic and public hospital EM physicians is significantly lower than those in the private sector. Consequently, many government and academic physicians must moonlight at a private hospital to support themselves.
Conclusion
These interviews provide a glimpse of many exciting developments in EM around the globe and the complexities of integrating EC into a nation’s healthcare system. We hope that these stories will inspire members of the EMRA community to continue engaging in collaborative efforts to develop high-quality EC worldwide.
GEMS LP
If you are a medical student, resident, or attending who is interested in global emergency medicine (GEM), we encourage you to reach out to us at info.GEMSLP@gmail.com. We are always looking for motivated and passionate students to join our next cohort of mentees, as well as mentors to help guide them in their GEM journey.
References
- Doney MK, Macias DJ. Regional highlights in global emergency medicine development. Emergency Medicine Clinics. 2005;23(1):31-44. doi:10.1016/j.emc.2004.09.011
- Turkey IS. Countries Recognize Emergency Medicine as a Specialty. International Emergency Medicine Education Project. Published May 13, 2019. Accessed May 12, 2021. https://iem-student.org/2019/05/13/countries-recognize-emergency-medicine/
- Journal Rankings on Emergency Medicine. Scimago Journal & Country Rank. Accessed May 13, 2021. https://www.scimagojr.com/journalrank.php?category=2711
- Razzak, J., Usmani, M. F., & Bhutta, Z. A. (2019). Global, regional and national burden of emergency medical diseases using specific emergency disease indicators: analysis of the 2015 Global Burden of Disease Study. BMJ Global Health, 4(2). https://doi.org/10.1136/bmjgh-2018-000733
- Holliman CJ, Mulligan TM, Suter RE, et al. The efficacy and value of emergency medicine: a supportive literature review. Int J Emerg Med. 2011;4:44. doi:10.1186/1865-1380-4-44
- Mock C. WHA resolution on trauma and emergency care services. Inj Prev. 2007;13(4):285-286. doi:10.1136/ip.2007.016485