Flecainide overdose is a rare but serious toxic ingestion. Treatment includes the aggressive administration of sodium bicarbonate and a low threshold to initiate ILE or ECMO.
You are working a busy overnight with your senior resident and attending when a broken patch comes through on the radio:
We are en route with a 30-year old female in cardiac arrest...history of heart problems...ET tube secure, 5 rounds of epi...See you in 4 minutes.
Realizing the gravity of cardiac arrest in such a young patient, your attending readies the room for a prolonged and vigorous resuscitation. On arrival, the patient is being actively coded with chest compressions and endotracheal ventilation. EMS reports that the patient was potentially down for approximately 20 minutes before being found by family. As you review the electronic medical record, a handful of pill bottles are given to you that were found on scene, including flecainide and ondansetron. A quick review of the chart shows a previous history of peripartum cardiomyopathy, history of pulmonary embolism (PE) no longer on anticoagulation, and bipolar disorder. With that information in mind, you continue the resuscitation.
Clinical Course
Over the next 2 hours, the patient goes in and out of wide complex arrhythmias, including torsades de pointes and monomorphic ventricular tachycardia. Throughout this time you have maintained concern for massive PE given her history, but also electrolyte derangements and prolonged qT syndrome given the additional information of the anti-emetic. Overdose is also a major concern. Point-of-care labs during the resuscitation were significant for hypokalemia and acidosis. Return of spontaneous circulation (ROSC) is achieved and lost repeatedly amidst multiple rounds of epinephrine, magnesium, potassium, and defibrillation. Bedside ultrasound is essentially unremarkable save an enlarged heart, with no evidence of right ventricular strain, tamponade, or aneurysm.
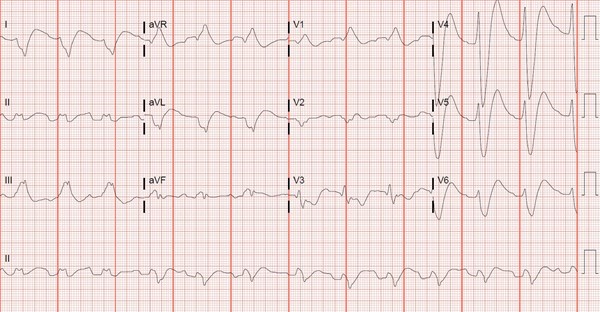
The family is insistent she was not suicidal, but given her heart's unresponsiveness to every medication in the code cart, you assume the worst and begin treatment for either accidental or intentional overdose. At this point you are able to achieve ROSC long enough to obtain an electrocardiogram.
About Flecainide Poisoning
Flecainide is a Vaughan Williams Class 1C antiarrhythmic. It works as a sodium channel blocker to prolong depolarization of myocytes and thus inhibit ventricular ectopy.1 As a sodium channel blocker, overdose can produce a characteristic EKG with a prolonged QRS, and a rightward axis which manifests most classically as a terminal R wave in aVR; ventricular tachycardia is also characteristic.2 QRS is usually 50% wider, PR is 30% prolonged, and QTc is 15% prolonged, producing an EKG characteristic of flecainide toxicity in particular.3
Clinically, toxicity can range from nausea and headache, to seizures and malignant dysrhythmias, to complete cardiovascular collapse. Treatment includes advanced cardiac life support, gastrointestinal decontamination, and aggressive administration of sodium bicarbonate. As with tricyclic overdose, sodium bicarbonate probably works to offset the sodium channel blocking effects of the drug, in addition to alkalinizing the serum and thus increasing the protein bound portion of flecainide as well as helping to dissociate the drug from myocytes.4
Refractory cases are not well studied in the literature, but a perusal of prior case reports reveals that frequent sodium bicarbonate boluses or infusion, intravenous lipid emulsion (ILE) administration, and extracorporeal membrane oxygenation (ECMO) are the mainstay, and show promising outcomes with the increasing availability of these modalities.5-8
Intravenous Lipid Emulsion Therapy
ILE is thought to work via a twofold mechanism: acting as a "lipid sink," thus sequestering the drug within the emulsion, and as source of fatty acids for poisoned myocytes.9 Dosing varies, but the American College of Medical Toxicology recommends a loading dose of 1.5 mL/kg pushed over 2-3 minutes, which can be repeated, followed by a 0.25 mL/kg/min infusion over an hour.10 Maximum dosing is approximately 10-12 mL/kg.11
The adverse effects of ILE include Lipid Overload Syndrome, which is characterized by headache, fever, liver toxicity, coagulopathy, and anemia.12 It also interferes with lab analysis and can cause spurious results on both blood counts and electrolytes, so efforts ought to be made to collect labs prior to administration.13 In addition, ILE is associated with fat deposition and clotting in ECMO circuits, leading to circulatory machine failure; however, ILE is not an absolute contraindication to ECMO. 14
When choosing treatment modality for a poisoned patient, clinicians have to take into consideration the stability of patient and availability of ILE and ECMO in the hospital.
Finally, there is some evidence that ILE alters the hemodynamic response to vasoactive agents, and patients in shock receiving ILE may need higher-than-expected doses of vasopressors to achieve goal blood pressures.15
Case Conclusion
The patient was given a 1.5 mL/ kg bolus of ILE twice, resulting in near instantaneous resolution of wide complex into a sinus rhythm. An infusion of the drug was started along with maximized vasopressor support, and the patient was transferred to the cardiac intensive care unit in stable condition but with a guarded prognosis. Unfortunately, the patient had already suffered devastating anoxic brain injury prior to the resuscitation, and care was withdrawn later on hospital day 1, with the patient quickly dying thereafter.
We had drawn a flecainide level in the ED just prior to giving the ILE, which resulted later as a whole blood concentration of 2.01 mcg/mL, more than double the upper limit of normal. Family who had later brought the patient's pill bottles from home noted only 10-15 tablets of flecainide missing, which is suggestive of the drug's narrow therapeutic window.
TAKE-HOME POINTS
- Flecainide overdose is a rare but serious toxic ingestion.
- Antiarrhythmic overdose should be considered in refractory cardiac collapse in otherwise healthy individuals or in those with access to these medications, in addition to anyone with a characteristic ECG.
- Treatment includes the aggressive administration of sodium bicarbonate and a low threshold to initiate ILE or ECMO.
References
1. Holmes B, Heel RC. Flecainide. A preliminary review of its pharmacodynamic properties and therapeutic efficacy. Drugs. 1985 Jan;29(1):1-33.
2. Wolfson AB ed. Harwood Nuss’ Clinical Practice of Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015:1449.
3. Nelson, Lewis S.. "Antidysrhythmics." Goldfrank's Toxicologic Emergencies, 10e. Eds. Robert S. Hoffman, et al. New York, NY: McGraw-Hill; 2015.
4. Bou-Abboud E, Nattel S. Relative role of alkalosis and sodium ions in reversal of class I antiarrhythmic drug-induced sodium channel blockade by sodium bicarbonate. Circulation. 1996 Oct 15;94(8):1954-61.
5. Vu NM, Hill TE, Summers MR, Vranian MN, Faulx MD. Management of life-threatening flecainide overdose: A case report and review of the literature. HeartRhythm Case Rep. 2015 Dec 29;2(3):228-231.
6. Brumfield E, Bernard KR, Kabrhel C. Life-threatening flecainide overdose treated with intralipid and extracorporeal membrane oxygenation. Am J Emerg Med. 2015 Dec;33(12):1840.
7. Ellsworth H, Stellpflug SJ, Cole JB, Dolan JA, Harris CR. A life-threatening flecainide overdose treated with intravenous fat emulsion. Pacing Clin Electrophysiol. 2013 Mar;36(3):e87-9.
8. Devin R, Garrett P, Anstey C. Managing cardiovascular collapse in severe flecainide overdose without recourse to extracorporeal therapy. Emerg Med Australas. 2007 Apr;19(2):155-9.
9. Rose SR, Stromberg PE. Antidysrhythmic Drugs and Local Anesthetics. In: Wolfson AB ed. Harwood Nuss’ Clinical Practice of Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015:1400.
10. American College of Medical Toxicology. ACMT position statement: interim guidance for the use of lipid resuscitation therapy. J Med Toxicol. 2011 Mar;7(1):81-2.
11. Weinberg G. LipidRescue Resuscitation. lipidrescue.org. Updated February 11, 2010. Accessed January 15, 2019.
12. Hayes BD, Gosselin S, Calello DP, et al. Systematic review of clinical adverse events reported after acute intravenous lipid emulsion administration. Clin Toxicol (Phila). 2016 Jun;54(5):365-404.
13. Grunbaum AM, Gilfix BM, Hoffman RS, et al. Review of the effect of intravenous lipid emulsion on laboratory analyses. Clin Toxicol (Phila). 2016;54(2):92-102.
14. Lee HM, Archer JR, Dargan PI, Wood DM. What are the adverse effects associated with the combined use of intravenous lipid emulsion and extracorporeal membrane oxygenation in the poisoned patient? Clin Toxicol (Phila). 2015 Mar;53(3):145-50.
15. Carreiro S, Blum J, Jay G, Hack JB. Intravenous lipid emulsion alters the hemodynamic response to epinephrine in a rat model. J Med Toxicol. 2013 Sep;9(3):220-5.