Female hypospadias is an exceedingly rare congenital anomaly that can cause obstructive acute urinary retention in a few isolated cases.
Acute urinary retention (AUR) is a frequent urologic complaint in the adult emergency department with a broad differential including obstructive processes, medication side effects, infections, and neurologic dysfunction.1,2 Female hypospadias is an exceedingly rare congenital anomaly that can cause obstructive AUR with few isolated cases reported in the literature.3,4 We present a female patient with the chief complaint of AUR who presented to the emergency department with hypospadias.
Case
A 32-year-old female visiting from out of state with a history of recurrent urinary tract and vaginal infections presented to our emergency department with a complaint of urinary retention. She woke up in the morning unable to void and after a few hours developed significant suprapubic discomfort. She reported one similar episode of urinary retention four months prior that required catheter placement.
On initial evaluation, she appeared uncomfortable and was tachycardic to the 130s with otherwise unremarkable vitals. The patient reported she was in the process of being evaluated further by a urologist for her recurrent genitourinary infections and had recently been told her urethra was located inside the vagina. Nurses attempted to place a Foley catheter but were unable to successfully locate the urethra. A speculum was used to fully visualize the vaginal canal in an attempt to catheterize the patient. After being unable to locate any urethral opening, the speculum was rotated sideways, which allowed visualization of the anterior vaginal wall. An orifice was then identified - suspected to be the urethral meatus - approximately 2.5 cm from the introitus in the anterior wall in the vagina.
A Foley catheter was successfully placed through the urethra with subsequent return of clear urine and immediate patient relief. The patient’s tachycardia resolved after bladder drainage. A urinalysis showed rare bacteria. Additional workup for urinary retention in this patient was not performed due to known history of urogenital structural abnormality and previously established care with urology. The patient was offered a urinary leg bag because she was scheduled to travel to her home state later that day. She refused and agreed to seek medical attention if she developed recurrent retention. She was discharged and encouraged to follow up with her urologist for definitive management of her urethral abnormality.
Discussion
In female patients, the two most frequent causes of AUR are obstruction or inherent dysfunction of the bladder.1 Undiagnosed congenital urethral abnormalities are a rare cause of AUR that have the potential to result in severe renal complications.4 The prevalence of hypospadias is, not surprisingly, much higher in males than females with an estimated ratio of 150:1.5 Female hypospadias is thought to be caused by a failure of appropriate urogenital fusion, and most patients with female hypospadias have additional genitourinary abnormalities.6,7
The diagnosis of isolated female hypospadias is extremely rare and most often made incidentally during difficult catheterizations for unrelated events such as surgical procedures.4 The most common problems that arise in patients with isolated female hypospadias include repeated urinary and vaginal infections.5 These infections typically become recurrent after the patient begins engaging in sexual intercourse and are likely related to the urethral position in the vagina [4]. Other rare complications have been reported including one patient who was found to have vaginal stones, possibly due to longstanding pooling of urine in the vaginal canal.5
In female patients with hypospadias, the severity of outflow obstruction varies depending on the location of the urethral meatus.8 Urethral diameter is more likely to be significantly constricted in patients with a meatus located in the upper two-thirds of the vagina.8 Because of this, patients with a urethra located more proximally inside the vaginal canal are more likely to present during childhood or adolescence due to an increased probability of developing severe obstructive retention.7 Our patient’s urethra was located in the distal third of the vagina, which may have contributed to her delayed diagnosis as an adult. The patient’s recurrent urinary and vaginal infections without prior reported history of severe renal complications also led us to confirm isolated female hypospadias.
Regardless of etiology, the standard treatment for patients who present to the emergency department with urinary retention is bladder decompression.2 Female patients with hypospadias are difficult to catheterize for a few reasons. In addition to inherent difficulty locating a true urethral meatus, recurrent infections and repeated catheterization attempts in these patients may predispose them to urethral stenosis. If attempts at urethral catheterization are unsuccessful, patients require a suprapubic catheter. Once the bladder is drained, unless there are additional renal complications that need to be addressed, the patient can be safely discharged and managed outpatient with prompt urology follow-up.2 Surgical correction is the only definitive treatment for this condition.4,6
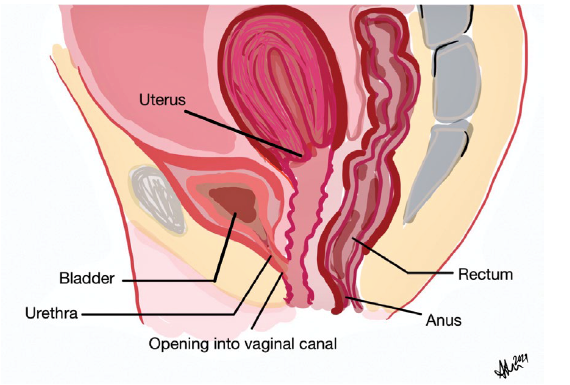
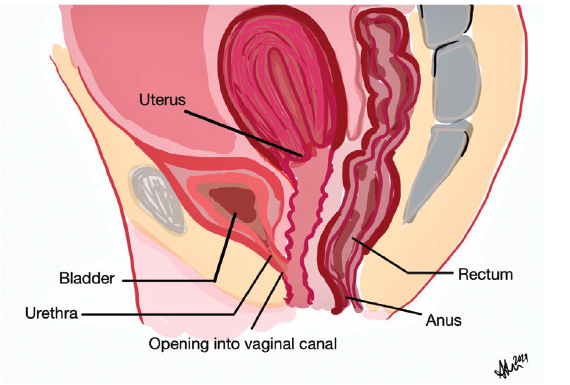 FIGURE 1. Representative drawing of isolated female hypospadias
FIGURE 1. Representative drawing of isolated female hypospadias
In isolated female hypospadias, the urethra opens directly into the vaginal canal.
Conclusion
Patients with urethral abnormalities should be evaluated by urology for definitive management because of the high probability of future complications. Women with urethral anomalies who present during adolescence or later in adulthood with dyspareunia and recurrent genitourinary infections are more likely to have true isolated hypospadias, which is extremely rare.7 Because isolated female hypospadias may remain asymptomatic for years, it is likely that many patients may initially be diagnosed in the emergency department. Emergency medicine physicians should be aware of this anomaly and may have to utilize unconventional methods to identify the urethra in these patients. If presenting with urinary retention, it may be helpful to ultrasound the bladder once a foley has been inserted to confirm appropriate placement.
This diagnosis may also be considered in patients who present with recurrent urinary tract infections that do not respond to antibiotics.5 It is a condition that is especially relevant for specific patient populations that may not have had access to thorough neonatal physical exams, and should also be considered in pediatric patients who present with recurrent urinary tract infections or urinary retention.
The progression of our patient’s symptoms reinforces the need for definitive management of any patient with congenital urethral abnormalities. Emergency medicine physicians should ensure that all patients with this diagnosis establish prompt follow-up care with urology to prevent worsening urogenital symptoms and future complications.
References
- Dougherty JM, Rawla P. Female Urinary Retention. 2021 Mar 29. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 30860732.
- Billet M, Windsor TA. Urinary Retention. Emerg Med Clin North Am. 2019 Nov;37(4):649-660. doi: 10.1016/j.emc.2019.07.005. Epub 2019 Aug 16. PMID: 31563200.
- Fischelovitch J, Ben-Bassat M. Female hypospadias. Br J Urol. 1976 Feb;48(1):72. doi: 10.1111/j.1464-410x.1976.tb02745.x. PMID: 1268468.
- Prakash G, Singh M, Goel A, Jhanwar A. Female hypospadias presenting with urinary retention and renal failure in an adolescent: uncommon and late presentation with significant hidden morbidity. BMJ Case Rep. 2016 Sep 22;2016:bcr2016215064. doi: 10.1136/bcr-2016-215064. PMID: 27659910; PMCID: PMC5051457.
- Bhat A, Saxena R, Bhat MP, Dawan M, Saxena G. Female hypospadias with vaginal stones: a rare congenital anomaly. J Pediatr Urol. 2010 Feb;6(1):70-4. doi: 10.1016/j.jpurol.2009.03.014. Epub 2009 Apr 26. PMID: 19394897.
- Bavadiya G, Shah C, Sarkar KK, Ghoshal P, Pathak H, Sarkar K. Unusual presentation of female bladder outlet obstruction- female hypospadias with urethral stenosis. Urol Case Rep. 2020 May 8;32:101243. doi: 10.1016/j.eucr.2020.101243. PMID: 32455118; PMCID: PMC7235932.
- Sarin YK, Kumar P. Female Hypospadias-Need for Clarity in Definition and Management. J Indian Assoc Pediatr Surg. 2019 Apr-Jun;24(2):141-143. doi: 10.4103/jiaps.JIAPS_69_18. PMID: 31105404; PMCID: PMC6417043.
- Knight HM, Phillips NJ, Mouriquand PD. Female hypospadias: a case report. J Pediatr Surg. 1995 Dec;30(12):1738-40. doi: 10.1016/0022-3468(95)90469-7. PMID: 8749941.