In the United States, more than 350,000 out-of-hospital cardiac arrests occur each year.
One-third present to ambulance services with ventricular fibrillation (VF) or pulseless ventricular tachycardia.1 VF is often the result of significant left coronary artery disease (>70% stenosis),2 and there is a dismal survival rate of 8-15% when refractory to treatment.3 Cardiac catheterization can provide definitive treatment, however, patients often die before reaching the cardiac catheterization lab. ECPR involves the application of percutaneous veno-arterial extracorporeal membrane oxygenation (VA-ECMO) for management of cardiac arrest in the emergency department. ECPR functions as a bridge therapy, enabling temporary systemic organ perfusion until the cause of cardiac failure can be definitively treated. We present a case of ECPR-enabled cardiac stenting and post-arrest care, leading to a full neurological recovery in a patient who otherwise may not have survived refractory VF.
Case Report
A 54-year-old man walked into the emergency department waiting room complaining of chest pain. Suddenly, he collapsed into the arms of a triage nurse and turned ashen gray and unresponsive as he was hoisted onto a stretcher and wheeled back to the resuscitation bay. Cardiopulmonary resuscitation (CPR) began promptly when the team was unable to palpate a pulse. Per brief history from the patient’s wife, he had developed chest pain early in the day and drove himself to the emergency department. He had a history of hypertension and no prior cardiac disease.
Cardiac monitoring revealed ventricular fibrillation and the patient was defibrillated with 200 joules while resuscitation efforts began. During the first several minutes of resuscitation, the patient drifted in and out of consciousness, pushing away CPR providers as he did. This is a phenomenon described in medical literature as cardiopulmonary resuscitation-induced consciousness (CPRIC), an indicator of good cerebral perfusion and CPR.4 With each sign of CPRIC, compressions were immediately stopped and pulse checks were performed. However, there was no palpable pulse and the patient lost consciousness shortly after cessation of CPR. He received multiple defibrillations, epinephrine, and amiodarone. He was intubated, and an EKG (Figure 1) confirmed ventricular fibrillation. A second set of defibrillation pads were placed in the anterior-posterior position for dual synchronous defibrillation. This patient was in refractory ventricular fibrillation and a call was made to evaluate the patient for ECPR. The cardiothoracic surgical team began cannulation 52 minutes after cardiac arrest, and full flow VA-ECMO was achieved 58 minutes post-arrest.
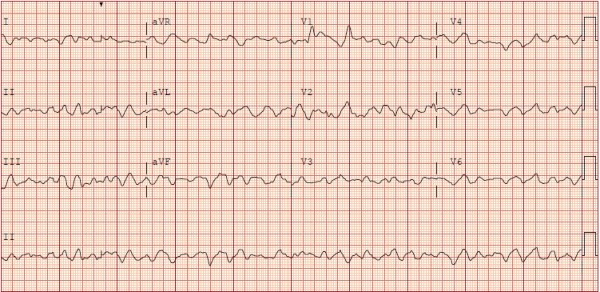
Figure 1
Due to a high suspicion for ischemia-mediated dysrhythmia, the patient was emergently transported to the cardiac catheterization laboratory where coronary angiography confirmed a 99% occlusion of the left anterior descending artery. This “widowmaker” lesion was successfully treated with one drug-eluting stent, and the left ventricle was decompressed with placement of an Impella (Abiomed, Danvers, MA, USA). Following revascularization, defibrillation was performed with successful and durable conversion to normal sinus rhythm. The patient was admitted to the cardiothoracic intensive care unit for post-arrest care. The VA-ECMO circuit enabled targeted temperature management for the first 24 hours. Echocardiography revealed severe left ventricular dysfunction with an ejection fraction of 10-15%. The Impella enabled ventricular decompression, allowing the myocardium to rest and recover. On day three, repeat echocardiography showed a recovered ejection fraction of 45% and the patient was successfully decannulated. The patient’s care continued in the medical intensive care unit where he returned to his pre-arrest neurological baseline and was discharged home.
Discussion
What are the indications for ECPR?
ECPR is a bridge therapy for patients with cardiac arrest refractory to ACLS. ECMO has been employed in a range of cardiac and respiratory failure patients with reversible etiologies; e.g. obstructive coronary artery disease, massive pulmonary embolism, COVID-19, acute respiratory distress syndrome, hypothermia, electrolyte derangements, cardiotoxicity due to drug overdose, and submersion injuries.5 VA-ECMO and more specifically, ECPR, has been used and studied predominantly in VF, caused by left heart disease in 87% of cases.2 When VF is refractory to traditional advanced cardiac life support, the survival rate is extraordinarily low (8-15%).3 While clinical gestalt, experience and team readiness continues to play a large role in present day application, ECPR indications include: young age, witnessed arrest, bystander CPR, initial shockable rhythm, correctable causes such as a cardiac etiology, and no return of spontaneous circulation within three defibrillations.6 Patients in refractory ventricular fibrillation often have reversible etiologies and represent a large population who benefit from well-developed ECPR programs.
Which patients are ideal candidates for ECPR?
ECPR should be considered for patients in cardio-pulmonary arrest with both a reversible etiology and a high likelihood of return to a comparable neurological baseline. Ideal candidates are younger in age and have fewer comorbidities, witnessed cardiac arrest, shockable initial rhythm on cardiac monitoring, brief down-time, and brief time to cannulation. These variables factor into the SAVE score, a tool developed and externally validated to predict survival for patients receiving ECMO for refractory cardiogenic shock.6 Studies in the last decade have shown up to 54% survival rates with full neurological recoveries in out-of-hospital cardiac arrest patients in refractory VF.7,8 Most recently, The University of Minnesota completed the ARREST trial, a small RCT to evaluate ECPR versus standard ACLS.9 The trial was stopped early when clear benefit was observed in the ECPR arm versus standard ACLS. While small, this is the first RCT to evaluate the efficacy of ECPR over standard of care. Contraindications in the literature, while not absolute, include patients with poor physical activity levels, permanent neurological injury, noncardiac cause of arrest, prolonged CPR without return of spontaneous circulation, and aortic injury such as dissection.6
What times matter in ECPR resuscitation?
Favorable neurological outcomes with ECPR are achieved by minimizing downtime, known as no-flow, and time to cannulation, known as low-flow. Out-of-hospital arrests that are witnessed and have prompt initiation of bystander CPR minimize no-flow time and have better outcomes. The literature highlights optimal outcomes when no-flow is less than five minutes, and low-flow is less than 60 minutes.10 Few institutions have even developed mobile ECPR centers with a goal of under 30 minutes from arrest to cannulation.11
How does the heart recover?
VA-ECMO helps stabilize patients with cardiogenic shock, however, there are significant physiological changes that occur due to the retrograde flow towards the aortic valve. This physiologic alteration elevates afterload pressures that the injured ventricle must overcome. Ventricular over-distension can cause pulmonary edema, stasis, arrhythmias, and increased wall stress and myocardial oxygen demands. Subendocardial ischemia worsens LV function and recovery.12, 13 To prevent ventricular over-distension, clinicians recommend left ventricular venting using medical therapy, a surgical vent, or a percutaneous ventricular assist device. These devices, such as the intra-aortic balloon pump, Impella, or TandemHeart, optimize flow and enable myocardial recovery. In this patient, myocardial recovery occurred within the first three days and the patient was able to be safely decannulated with an ejection fraction of 45%. Per analysis of the Extracorporeal Life Support Organization registry, there is an increasing chance of survival up to four days, then a decreasing chance to day twelve. Thus, patients that survive the early period are more likely to survive if weaned shortly thereafter. Three quarters of patients receive treatment for less than one week.14
Conclusion
ECPR can be a life-saving therapy in refractory ventricular dysrhythmias. This case report provides an example of successful implementation of ECPR from the prehospital arena to the intensive care unit. We believe this report can serve as an introduction for providers who wish to better understand ECPR, and for emergency departments developing multi-disciplinary ECPR pathways.
References
- Daya MR, Schmicker RH, Zive DM, et al. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108-115.
- Yannopoulos D, Bartos JA, Raveendran G, et al. Coronary Artery Disease in Patients With Out-of-Hospital Refractory Ventricular Fibrillation Cardiac Arrest. J Am Coll Cardiol. 2017;70(9):1109-1117.
- Bartos JA, Carlson K, Carlson C, et al. Surviving refractory out-of-hospital ventricular fibrillation cardiac arrest: Critical care and extracorporeal membrane oxygenation management. Resuscitation. 2018;132:47-55.
- Olaussen A, Shepherd M, Nehme Z, Smith K, Bernard S, Mitra B. Return of consciousness during ongoing cardiopulmonary resuscitation: A systematic review. Resuscitation. 2015;86:44-48.
- ECMO Registry of the Extracorporeal Life Support Organization (ELSO), Ann Arbor, Michigan, June, 2020.
- Schmidt M, Burrell A, Roberts L, et al. Predicting survival after ECMO for refractory cardiogenic shock: the survival after veno-arterial-ECMO (SAVE)-score. Eur Heart J. 2015;36:2246–56.
- Stub D, Bernard S, Pellegrino V, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation. 2015;86:88-94.
- Shinar Z, Plantmason L, Reynolds J, et al. Emergency Physician-Initiated Resuscitative Extracorporeal Membrane Oxygenation. The Journal of Emergency Medicine. 2019;56(6):666-673.
- Yannopoulos D, Bartos J, Raveendran G, Walser E. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020;396(10265):1807-1816.
- Patricio D, Peluso L, Brasseur A, et al. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: a retrospective propensity score matched study. Critical care. 2019 Jan 28;23(1):27.
- Bartos JA, Frascone RJ, Conterato M, et al. The Minnesota mobile extracorporeal cardiopulmonary resuscitation consortium for treatment of out-of-hospital refractory ventricular fibrillation: Program description, performance, and outcomes. Lancet. 2020;29-30:100632.
- Al-Fares AA, Randhawa VK, Englesakis M, et al. Optimal Strategy and Timing of Left Ventricular Venting During Veno-Arterial Extracorporeal Life Support for Adults in Cardiogenic Shock. Circulation: Heart Failure. 2019;12(11).
- Truby LK, Takeda K, Mauro C, et al. Incidence and Implications of Left Ventricular Distention During Venoarterial Extracorporeal Membrane Oxygenation Support. ASAIO Journal. 2017;63(3):257-265.
- Smith M, Vukomanovic A, Brodie D, Thiagarajan R, Rycus P, Buscher H. Duration of veno-arterial extracorporeal life support (VA ECMO) and outcome: an analysis of the Extracorporeal Life Support Organization (ELSO) registry. Critical Care. 2017;21(1).



