A frail, elderly female presents after a ground-level fall with chest wall pain. Her trauma evaluation reveals T8 - T9 posterior rib fractures, and you note that she takes cyclobenzaprine as needed for chronic back pain. The patient receives morphine, but the nurse comes to you several times asking for more pain medications. You understand the importance of pain control in rib fractures, but are also concerned about opiate induced respiratory depression. What can you do to safely control her pain and possibly discharge her home?
Background
Rib fractures are common injuries, often occurring following blunt thoracic trauma. Approximately 10% of blunt trauma patients are found to have rib fractures, which can be associated with significant morbidity and mortality.1 Elderly patients are particularly susceptible to associated complications with pneumonia rates as high as 31%.1 Providing effective analgesia helps to prevent these complications, ICU stays, and even death. Opioids are usually the mainstay of treatment, however their side effects of respiratory depression, cough suppression, and delirium also contain risk for complications.4 Using regional anesthesia for the treatment of rib fractures has been shown to improve pulmonary function, including tidal volume and inspiratory force, and overall clinical outcomes when compared to treatment with opioids.5 In this article, we describe one regional nerve block that is particularly safe and effective in treating pain associated with rib fractures, the erector spinae plane block.
Procedure
The erector spinae plane is located just posterior to the spinous transverse processes and anterior to the erector spinae muscles. The erector spinae plane block (ESPB) primarily targets the dorsal and ventral rami of the thoracic spinal nerves, providing pain relief to the posterior chest wall via the former and to the anterolateral chest wall and injured periosteum via the latter.6 Whereas the serratus anterior block covers only anterolateral chest wall pain, the ESPB is able to cover the posterior thorax as well.
The ESPB uses standard nerve block supplies, which includes a 25-27 gauge needle for local anesthetic and a standard 20 gauge block needle. If a block needle is not available, a Quincke tip lumbar puncture needle will work as well. We recommend a preparation of 30 mL of 0.25% bupivacaine (2 mg/kg max) to allow adequate spread of the anesthetic within the fascial plane.
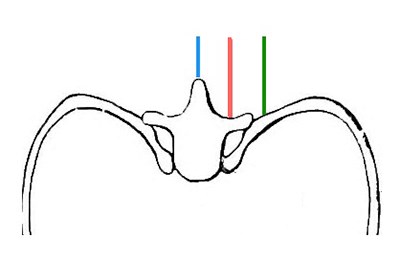
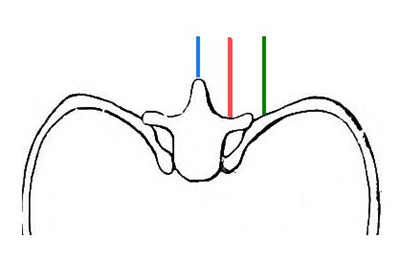
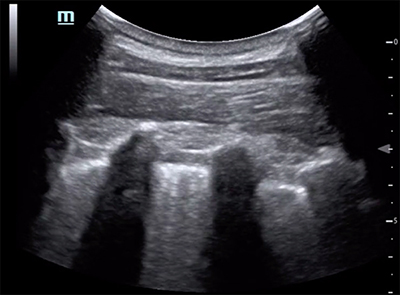
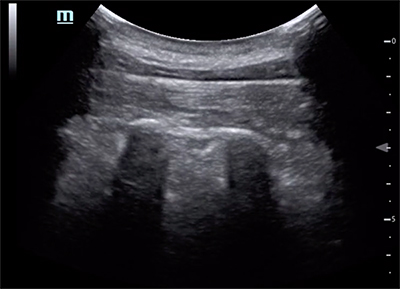
While a high frequency linear array transducer is generally better for high resolution images, in our experience the curvilinear transducer obtains better visualization of the important bony structures in overweight and obese patients. (See Image 1)
Image 1: Three sonographic planes to visualize.
To begin the procedure, position the patient in a sitting or lateral decubitus position with the unaffected side against the bed and establish your sterile field.
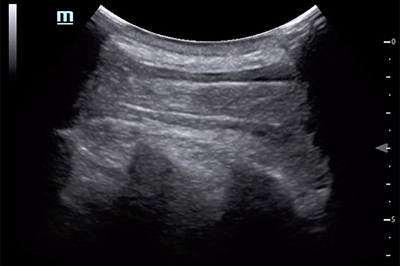
Start with the transducer in midline sagittal orientation to identify the thoracic spinous processes, which appear triangular like shark fins (Image 2).
Image 2: At the midline, the spinous processes appear triangular or like shark fins.
Slowly move the probe laterally about 2 - 3 cm to visualize the transverse processes, which appear as elongated ovoid structures (Image 3a).
Image 3a: The thoracic transverse processes have a gentle curvilinear contour. This is the target goldilocks zone.
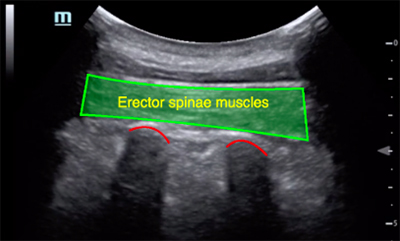
The erector spinae muscles and trapezius/rhomboid muscles lie directly above these transverse processes (Image 3b).
Image 3b: The erector spinae plane is located between these erector spinae muscles and transverse processes.
As the probe continues to move laterally beyond this target goldilocks zone, the more superficial, circular ribs and underlying pleura come into view clearly (Image 4).
Image 4: The ribs appear more superficial and rounded.
After landmarks and transverse processes are clearly identified, anesthetize the procedure site with a small wheal of local anesthetic before inserting the sturdier procedure needle in a cephalad to caudad direction. Target the injection to the plane just above the transverse process and below the erector spinae muscle, staying above the rib at all times to avoid creating a pneumothorax. Beginners may inject a small 1-2 mL aliquot of normal saline or anesthetic to confirm needle tip placement and hydrodissect fascial layers.
After the fascial layers open smoothly, slowly inject the anesthetic. As the anesthetic is injected, the erector spinae muscles should lift away from the transverse processes, revealing the erector spinae plane and neighboring transverse processes. We recommend waiting about 30 minutes to evaluate the full efficacy of this block.
The advantage of a ESBP is that the site of injection is distant to pleura, major blood vessels, and the spinal cord so there are relatively few contraindications. In addition, the local anesthetic spreads cranio-caudally along the fascial plane, providing pain relief to multiple vertebral levels with a single injection.
Absolute contraindications include allergy to local anesthetics, active overlying skin infection, or patient refusal. It is advised to reconsider or postpone injection in patients with pre-existing neurologic deficits along distribution of the block and in patients with coagulopathies.3
Case Conclusion
An ultrasound-guided ESPB is successfully performed and half an hour later the patient is able to breathe and move comfortably. She is amenable to discharge home with an incentive spirometer and does not require admission.
References
1. Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib Fractures in the Elderly. J Trauma. 2000;48(6):1040-1047.
2. Bergeron E, Lavoie A, Clas D, et al. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54:478-485.
3. Chang A, White BA. Peripheral Nerve Blocks. StatPearls [Internet]., U.S. National Library of Medicine, 3 May 2019. Available at: www.ncbi.nlm.nih.gov/books/NBK459210/.
4. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg Anesth Pain Med. 2016;41(5):621-627.
5. May L, Hillermann C, Patil S. Rib fracture management. BJA Educ. 2016;16(1):26-32.
6. Luftig J, Mantuani D, Herring AA, et al. Successful emergency pain control for posterior rib fractures with ultrasound-guided erector spinae plane block. Am J Emerg Med. 2018;36(8);1391-1396.