Eye-related emergencies make up close to 2% of all emergency department (ED) visits in the United States.1
For emergency physicians, the priority is to recognize and manage time-sensitive, vision-threatening diagnoses, and ensure appropriate management once the emergencies are ruled out. This is a case report of an uncommon diagnosis masquerading as a vision-threatening emergent eye complaint.
CASE REPORT
A 60-year-old male presents to the ED with worsening left eye redness for the past 4 days with associated photophobia and blurred vision. One day prior to arrival, he began to feel pressure in the left eye and observed halos around objects. He denied nausea, vomiting, rashes, or headache. He denied recent trauma or surgery to the eye. He used saline drops and ibuprofen with minimal relief of his symptoms. Relevant history included an infection of the left eye as an infant with subsequent visual disturbances; however, his vision was worse than baseline on presentation to the ED. Additionally, the patient had similar symptoms a few years ago, which were treated with “eye drops,” but he could not recall the diagnosis or the medication given at that time. Although the patient did not have any active cold sores at the time of presentation, he did confirm a history of labial cold sores during subsequent outpatient follow-up.
Initial exam of the left eye was remarkable for 3+ injection of the sclera and conjunctiva, pain with extraocular movements, and a fixed, dilated pupil at 5mm. The left eye also had severely reduced visual acuity and an intraocular pressure (IOP) of 20mmHg. The right eye exam was unremarkable. Despite the IOP being within normal range, there was a high suspicion of acute angle closure glaucoma (AACG) and ophthalmology was immediately consulted. As the team was in-house and findings were inconsistent with glaucoma, initiating treatment in the ED was deferred. Per ophthalmology, visual acuity was 20/800 -1 in the left eye. The slit lamp exam of the left eye revealed decreased corneal sensation, diffuse corneal edema including Descemet's folds, iris posterior synechiae, and anterior chamber cells. The anterior chamber of the left eye was deep. Posterior segment exam was unremarkable for both eyes with normal optic nerve and retinal findings.
Given the anterior chamber inflammatory reaction with the presence of corneal edema and absence of corneal sensation, the diagnosis of endotheliitis likely secondary to herpes simplex virus (HSV) was made by ophthalmology. He was discharged with valacyclovir 500mg three times daily, prednisolone acetate 1% topical drops four times daily, and cycloplegic cyclopentolate 1% topical drops four times daily. Outpatient follow-up with a cornea specialist was scheduled for 2 days following the ED visit.
At the follow-up visit, the patient’s ocular pressures in the left eye were 19 and 21 mmHg, with scattered inferior keratic precipitates (KP) and improved corneal edema further confirming the diagnosis of HSV keratouveitis. The corneal edema and anterior chamber reaction resolved with a slow taper of the steroid eye drops and oral valacyclovir over the following 6 weeks.
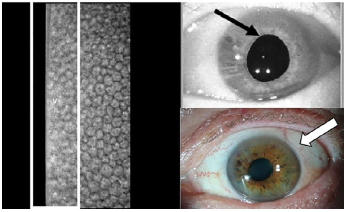
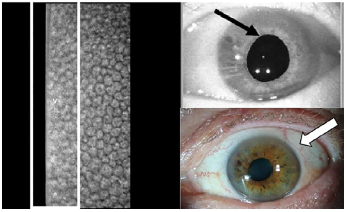
Image: Corneal endothelial cell electron specular microscopy and slit lamp images of the left eye obtained 2 days after initial presentation with herpes simplex virus keratouveitis. The white rectangle shows cell drop out and the white dots in the rectangle are keratic precipitates. The black arrow highlights the posterior synechiae, adhesions between the iris at the pupillary margin and anterior lens capsule that occur with inflammation, causing the pupil to be irregular and dilated. The white arrow shows the mild corneal edema.
The patient’s presentation of scleral and conjunctival erythema, severe eye pain, photophobia, decreased vision, and a dilated pupil raised concern for AACG. However, given the patient’s high-normal IOP, anterior chamber inflammation, and lack of anterior chamber shallowing, inflammatory causes were considered including HSV keratouveitis.
DISCUSSION
Herpes simplex virus keratouveitis is an uncommon presentation of an HSV ocular infection, and HSV contributes to about 5-10% of uveitis cases.2 Uvea refers to the middle part of the eye. The iris and ciliary body form the anterior portion of the uvea (Figure 1)3. Keratouveitis is inflammation of the cornea and anterior uvea. Symptoms include pain, blurry vision, photophobia and redness. Exam findings can include a combination of corneal epithelial and stromal edema, stromal keratitis, keratic precipitates, endotheliitis, and anterior chamber cells and flare.2 Endotheliitis is inflammation of the corneal endothelium. The endothelial layer is the innermost layer of the cornea with a specialized basement membrane called Descemet membrane. Folds in the Descemet membrane are caused secondary to severe corneal edema.4 Keratic precipitates are inflammatory cellular deposits on the corneal endothelium and can vary in form and location.2
A distinguishing factor for HSV keratouveitis from other causes is an increased IOP secondary to inflammation of the trabecular meshwork, or trabeculitis, which impacts aqueous flow.5 Other forms of uveitis typically have a low IOP as ciliary body inflammation leads to decreased aqueous humor production.6 In this case, the IOPs were on the higher side of normal, in direct contrast with the IOPs of AACG which tend to be much higher. This patient also had a non-reactive pupil which was due to formation of scarring on the posterior iris to the anterior lens capsule due to intraocular inflammation. Additionally, HSV keratouveitis has significant corneal edema compared to other etiologies.5 Treatment includes topical glucocorticoids and systemic antivirals.2
CONCLUSION
As demonstrated in this case, it is not only important to have a high suspicion of emergent diagnoses, but to also consider other diagnoses. As emergency physicians, we must perform a complete physical exam to consider all diagnoses and further differentiate them. In this case, the vitals of the eye (pupils, vision, and pressure) were essential and saved the patient from unnecessary glaucoma treatment. Appropriate management of the presenting complaint and early discussion with consultants, if available, can lead to a more focused exam and expedited diagnosis and treatment. If consultants are not available, proper bedside exam and early discussion can facilitate appropriate transfer to a higher level of care or timely outpatient follow up. Given early timing of treatment for this patient, his condition resolved with no decline in vision. If the patient had not received the necessary steroids and valacyclovir prior to discharge from the ED, his condition would have continued to worsen until his outpatient follow-up.
REFERENCES
- Channa, R., Zafar, S. N., Canner, J. K., Haring, R. S., Schneider, E. B., & Friedman, D. S. (2016). Epidemiology of Eye-Related Emergency Department Visits. JAMA Ophthalmol,134(3),312-319.
- Gritz, D. C. (2021, February 24). Herpes Simplex Uveitis. EyeWiki. https://eyewiki.aao.org/Herpes_Simplex_Uveitis.
- Rosenbaum, JT. Uveitis: Etiology, Clinical Manifestations, and Diagnosis. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA, 2020.
- Dawson, D. G., & Edelhauser, H. F. (2010). Chapter 9 - Corneal edema. In L. A. Levin & D. M. Albert (Eds.), Ocular Disease (pp. 64-73). Edinburgh: W.B. Saunders.
- Morishige, N., Morita, Y., Yamada, N., & Sonoda, K. (2016). Differential Changes in Intraocular Pressure and Corneal Manifestations in Individuals With Viral Endotheliitis After Keratoplasty. Cornea, 35(5),602-606.
- Trottini, M., & Tolud, C. (2013, November 15). The Many Moods of Uveitis. Retrieved from https://www.reviewofoptometry.com/article/the-many-moods-of-uveitis