The treatment of geriatric trauma patients in the ED can be challenging because of concomitant medical pathology. Care of geriatric patients is further complicated by end of life wishes, which are often not immediately known.
This case describes a geriatric patient who presented as a critical trauma but was found to have a severe underlying medical issue. She was stabilized, and invasive resuscitation measures were avoided until her wishes were known. In this case we discuss anchoring bias in trauma patients and end of life care for geriatric patients in the ED.
Background
The number of geriatric patients who visit the ED is increasing. Many of these patients present as trauma activations, while also having serious medical conditions. It is important to avoid anchoring on a patient's "trauma" status in order to avoid missing important medical diagnoses. In this case, we discuss a geriatric patient who presented as a trauma; however, that trauma was mild and secondary to a more critical medical condition. We also discuss anchoring bias in trauma patients as well as end of life care for geriatric patients in the ED.
Case
A 90-year-old female presented as a critical trauma to the ED. The patient arrived via EMS, who reported that she fell at home and was found minimally responsive on the floor by her son. She was last seen normal 15 hours before presentation. EMS noted her to have signs of a head injury, hypotension, a Glasgow Coma Scale (GCS) of 9, and glucose of 49 mg/dL. EMS administered glucagon and 10% dextrose en route, with no change in mental status.
On arrival to the ED, vital signs were heart rate 65 bpm, blood pressure 84/49 mmHg, and oxygen saturation 90% on room air. The patient was responsive only to pain. The primary survey revealed she was extremely cold to the touch. Her exam was otherwise notable only for a parietal scalp laceration. The extended focused assessment with sonography in trauma (eFAST) was positive for bilateral pleural effusions.
Soon after, the patient became bradycardic to 32 bpm and was noted to be in complete heart block. The ED attending discussed with the trauma surgery attending that this was most likely a medical patient who fell, instead of a primary trauma patient. The trauma surgery attending deferred to the ED attending, who transitioned to medical resuscitation. The patient was given oxygen via non-rebreather mask, 50% dextrose, atropine, low dose intravenous epinephrine, bicarbonate, empiric antibiotics, peripheral norepinephrine infusion, and a Bair Hugger® was placed for hypothermia. The patient's pulse and blood pressure subsequently improved.
Laboratory work-up was notable for anemia, lactic acidosis, and elevated creatine phosphokinase (CPK) (Table 1). After stabilization, the patient was transported for imaging, where computed tomography (CT) of the head showed a small frontal hematoma and chest x-ray showed moderate bilateral pleural effusions (Figure 1). Additional CT imaging studies were obtained with no significant further findings. The patient's son arrived and provided information that the patient had a history of congestive heart failure and a pacemaker with an outdated battery and explained that his mother chose not to have the battery replaced. The son confirmed she did not desire any lifesaving intervention. The patient was then transitioned to comfort care, with the cessation of vasopressors and initiation of a fentanyl drip for pain, and was placed on hospice.
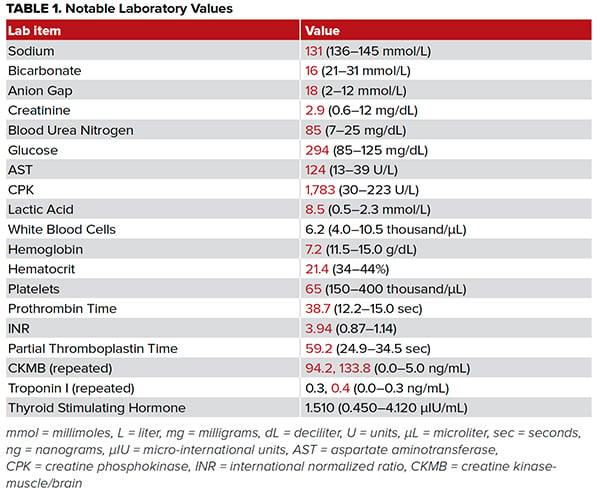
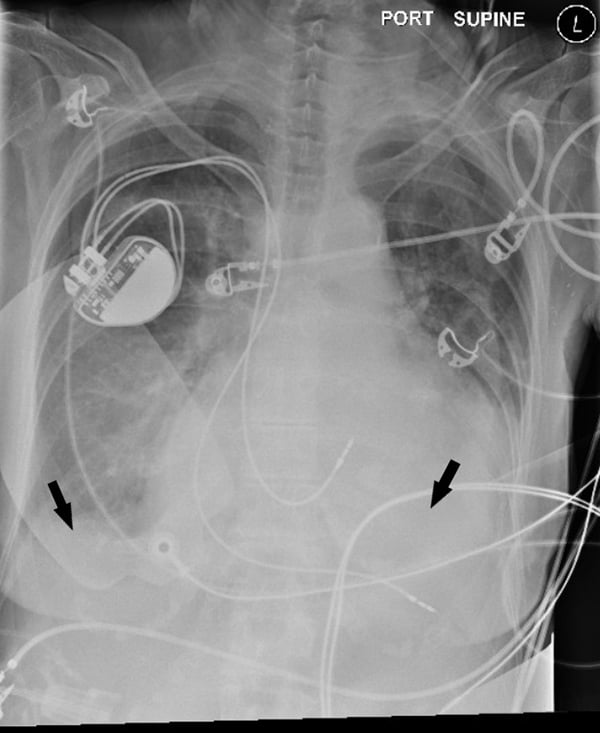
Figure 1. Chest x-ray showing bilateral pleural effusions (arrows)
Discussion
This case illustrates the importance of avoiding anchoring bias in designated trauma patients in the ED. The clinical environment of the ED makes the use of protocols and algorithms helpful; however, these tools can potentially contribute to cognitive biases.1–3 A common cognitive biases in medicine is the anchoring effect, in which the clinician fixates on a diagnosis based on initial presenting features, failing to adjust when new information becomes available.3–5 A situation in which emergency physicians are prone to anchoring bias is in trauma code activations. Trauma care has been noted to be particularly susceptible to medical error given the combination of unstable patients, incomplete information, and multiple medical services and providers working together.6 Additionally, trauma activations can be susceptible to anchoring bias because of the protocolized framework of trauma assessment and intervention. However, some of these pre-determined trauma patients may also have critical medical conditions that can be overlooked if the treatment team focuses exclusively on the patient as a trauma case. It is important that emergency physicians maintain a broad differential and direct the care team for the patient’s benefit as new information arises. In this case, it was quickly realized that the patient was not a critical trauma patient, but rather had serious medical conditions that likely led to a fall from standing. If the trauma protocol had been blindly followed, critical medical interventions may have been missed or severely delayed in order to follow protocol. This was averted by avoiding the inclination to anchor on the patient’s status as a trauma patient.
This case also highlights the value of considering end of life care in geriatric patients in the ED. Geriatric patients (age > 65) make up an increasingly large percentage of patients presenting to the ED, leading to an expanding role of emergency physicians in end of life discussions. This necessitates a focus on the ethics of resuscitation in geriatric patients.7 More than half of geriatric patients visit the ED in the last month of their life; of those, most will be admitted, and many will die in the hospital.8 Resuscitation of critically ill geriatric patients in the ED can be challenging both medically and ethically, as the principle of "do no harm" can be difficult for physicians to navigate, especially if the patient’s wishes are not immediately known.9 Numerous studies have found that geriatric patients resuscitated in the hospital have worse outcomes than younger patients, with a recent large study of geriatric patients intubated in the ED reporting that 33% died in the index hospitalization and only 24% were discharged home.10–12
With the risks of aggressive resuscitation in the elderly, it is important for emergency physicians to discover patients' end of life wishes. This task is complicated because the majority of geriatric patients do not have an advance directive upon presentation to the ED, they present to a hospital different than the hospital they normally utilize, and/or the patient is often not able to personally discuss their wishes.13 In the present case, the patient's end of life wishes were unknown, yet aggressive and unnecessary invasive measures were avoided. When her son arrived, he was able to confirm that the patient had an underlying severe medical disease and clarified the patient's end of life goals, allowing the physicians to honor the patient’s wishes. Because this case was approached conservatively, it was feasible to both stabilize the patient and respect her unknown wishes. Once the patient's wishes were verified, the patient was transitioned to comfort care and hospice placement.
Initiation of palliative measures in the ED has been shown to decrease length of stay, increase patient quality of life, and increase patient satisfaction.14 Though it is often challenging to identify candidates for these measures, when patient wishes are known, initiation of palliative measures increases the quality of care provided to these patients in the ED. This patient was able to be discharged home with her son, avoiding intubation and a stay in the intensive care unit.
Conclusion
One day after admission, the patient's condition had stabilized; however, the patient remained unresponsive. The patient was discharged home on full-time hospice care with her son.
Take-Home Points
- Be mindful of the tendency toward anchoring bias, especially in patients who arrive as trauma activations.
- When patient wishes are unknown, strongly consider the risks and benefits of aggressive resuscitation in geriatric patients, as aggressive resuscitation has been shown to lead to worse outcomes in the elderly population.
- When appropriate, seek to initiate end of life care measures in the ED, which has been shown to increase patient quality of life and improve patient experience.
Authors' disclosure: This research did not receive any specific grant from funding agencies in the public, commercial, or nonprofit sectors. Dr. Brinley Rajagopal has financial interests in Chromacode Inc., Esperto Medical Inc., Cardinal Health, and LunaPBC. Neither Dr. Roh nor Mr. Jasperse have any financial interests or other conflicts of interest to disclose.
References
- Bordini BJ, Stephany A, Kliegman R. Overcoming Diagnostic Errors in Medical Practice. J Pediatr. 2017;185:19-25.e1.
- Croskerry P, Sinclair D. Emergency medicine: A practice prone to error? CJEM. 2001;3(4):271-276.
- Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med. 2002;9(11):1184-1204.
- Saposnik G, Redelmeier D, Ruff CC, Tobler PN. Cognitive biases associated with medical decisions: a systematic review. BMC Med Inform Decis Mak. 2016;16(1):138.
- Famularo G, Salvini P, Terranova A, Gerace C. Clinical errors in emergency medicine: experience at the emergency department of an Italian teaching hospital. Acad Emerg Med. 2000;7(11):1278-1281.
- Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg. 2006;244(3):371-380.
- Samaras N, Chevalley T, Samaras D, Gold G. Older patients in the emergency department: a review. Ann Emerg Med. 2010;56(3):261-269.
- Smith AK, McCarthy E, Weber E, et al. Half of older Americans seen in emergency department in last month of life; most admitted to hospital, and many die there. Health Aff (Millwood). 2012;31(6):1277-1285.
- Perera T, Cortijo-Brown A. Geriatric Resuscitation. Emerg Med Clin North Am. 2016;34(3):453-467.
- van Gijn MS, Frijns D, van de Glind EM, C van Munster B, Hamaker ME. The chance of survival and the functional outcome after in-hospital cardiopulmonary resuscitation in older people: a systematic review. Age Ageing. 2014;43(4):456-463.
- Cooper S, Janghorbani M, Cooper G. A decade of in-hospital resuscitation: outcomes and prediction of survival? Resuscitation. 2006;68(2):231-237.
- Ouchi K, Jambaulikar GD, Hohmann S, et al. Prognosis After Emergency Department Intubation to Inform Shared Decision-Making. J Am Geriatr Soc. 2018;66(7):1377-1381.
- Oulton J, Rhodes SM, Howe C, Fain MJ, Mohler MJ. Advance directives for older adults in the emergency department: a systematic review. J Palliat Med. 2015;18(6):500-505.
- George NR, Kryworuchko J, Hunold KM, et al. Shared Decision Making to Support the Provision of Palliative and End-of-Life Care in the Emergency Department: A Consensus Statement and Research Agenda. Acad Emerg Med. 2016;23(12):1394-1402.



