On Jan. 2, Buffalo Bills safety Damar Hamlin, 24, suffered cardiopulmonary arrest on the field against the Cincinnati Bengals.
Reports showed that return of spontaneous circulation was achieved after approximately nine minutes of advanced cardiac life support. These nine minutes and their sequelae have traumatized Hamlin, his loved ones, and thousands of fans. They have also shed light upon the emotional toll of a daily occurrence for many of us in emergency medicine.
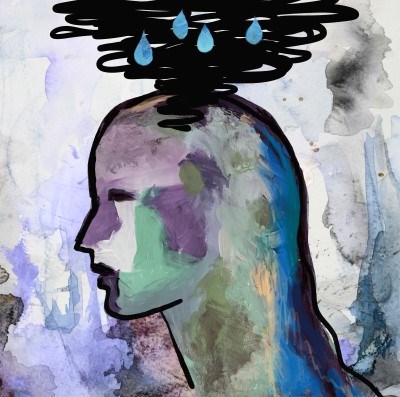
It's easy to forget that the majority of the population has never witnessed cardiopulmonary arrest. The natural response of shock and fear is one we have grown accustomed to through our line of work. While this ability to compartmentalize is an occupational necessity, it is prudent to acknowledge the emotional trauma throughput of even a single shift. Starting with the recognition that we, too, deserve safe spaces and time for human responses to the devastating situations we encounter will allow us to construct both individual and systematic safeguards against the cumulative effects of residency training and a subsequent career in the emergency department.
I started one of my shifts last week by taking care of a lovely woman in her 60s who was presenting with two days’ history of myalgia. She had completed a course of chemotherapy just two months prior and had been feeling well up until this week. On physical exam, there was left-sided weakness consistent with what her supportive husband had noticed over the past week. My developing clinical acumen gave me foresight for a right-sided frontotemporal mass, but still, I held my breath and hoped it would be influenza.
Later in the same shift, a woman in her 70s presented after she was found to be unresponsive by her family and hypoxic by EMS. We stabilized her and one of her sons arrived at bedside shortly after. His first words to me: “My father just died yesterday morning.” Within a span of 48 hours, this man and his brother fulfilled the responsibility of determining the code status of their critically ill mother — before they were able to finalize funeral plans for their father.
In writing this, I am hit with the realization I never properly reconciled the emotional effects of this shift. There must be better approaches than the one I take now, which, if I am being honest, is to try to not think of these patients again. Unfortunately, suppressing the emotional toll does nothing to diminish its effects because ... where else can the sadness go?
These experiences are why I appreciate Dr. Sian Lewis-Bevan’s vulnerability in sharing how residency has taught her to care for a breadth of clinical presentations, but the emotional cost has led to challenges in caring about both personal and professional components of life (“How to Care,” page 54).
Similarly, Dr. Adiba Matin eloquently highlights the bioethical implications and emotional difficulties associated with caring for patients who may not present so unfortunately end-of-life, but instead may have committed criminal acts (“The Ethics of Caring for an Unfavorable Patient,” page 44). These patients, too, are part of the emotional trauma throughput.
While there may never be a simple solution, I personally find that acknowledgement of these heavy subjects alleviates some of the burden and perhaps we, as a generation, can hold soft spaces to process the challenging situations we face each day. I consider it a privilege to read your fascinating cases, written with more nuanced and patient-centered language compared to the current literature. This time, I am even more touched to bear witness to brave and vulnerable acknowledgements of the ubiquitous emotional toll associated with residency training.