Case.
An 81-year-old female with a history of hypertension presents with episodes of lightheadedness.
What do you see in this 12-lead rhythm strip?
Note: The 3 images are continuous.
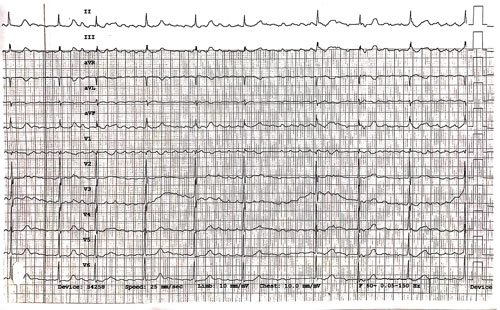
Image 1
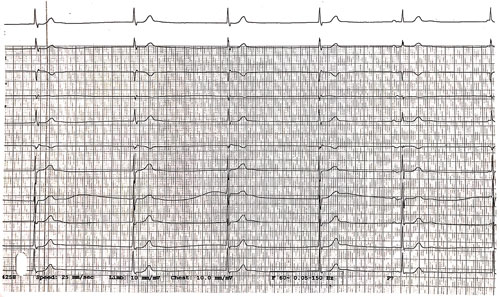
Image 2
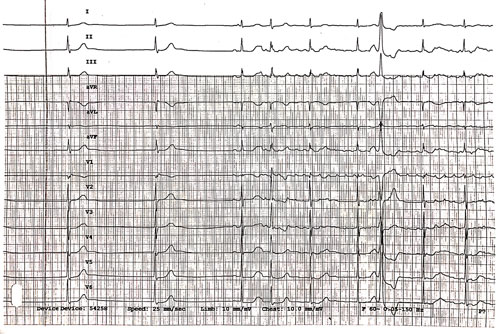
Image 3
Answer
Image 1. The initial rhythm is coarse atrial fibrillation (AFib) with an average ventricular rate ~60 bpm. It was initially mistaken for atrial flutter (AFlutter) with variable block because the large amplitude f-waves (fibrillatory waves) look like F-waves (flutter waves) and appear regular at ~300 bpm. However, AFlutter will demonstrate consistent F-wave morphology, duration, and timing with the absence of an isoelectric baseline in lead II. AFib is typically described as “coarse” when the majority of f-waves are easily seen and have an amplitude ≥3-5 mm.
| Atrial Fibrillation | Atrial Flutter | |
| General Features | Irregularly irregular rhythm with absence of any organized atrial activity
Presence of f-waves of varying morphology, duration, and timing |
Caused by a re-entrant circuit initiated in the right atrium
Stereotypical “sawtooth pattern” of F-waves best seen in the inferior leads |
| EKG Features | Absence of distinct repeating P-waves with atrial depolarization rate typically >300 bpm
Ventricular rates typically 100-200 bpm Irregular RR interval when AV conduction is present (ie, in the absence of a 3rd degree AV block) |
Atrial rate is 250-350 bpm and typically fixed over time
Ventricular rate is a fraction of atrial rate (2:1 → 150 bpm, 3:1 → 100 bpm) in the absence of a variable block Absence of isoelectric baseline |
| Clinical Significance | Rate <100 bpm in untreated AFib suggests significant AV node disease
Consider AFib with concurrent WPW when ventricular rate is > 250 bpm with wide QRS |
Consider AFlutter when ventricular rate is consistently around 150 bpm
Vagal maneuvers or adenosine will slow ventricular rate but not atrial rate |
Image 2. The rhythm changes to a junctional bradycardia at ~33 bpm.
There are likely retrograde P-waves after the QRS complexes in beats 1-4, best seen in V1 and aVR as upright deflections immediately following the QRS. Retrograde P-waves in these leads will usually be inverted (ie, upright, as they are typically inverted in normal sinus rhythm).
The 5th QRS complex is a sinus beat — narrow complex and preceded by a P-wave with a normal PR interval.
The 6th QRS complex is a junctional beat with a retrograde P-wave preceding the QRS with a PR interval <120 ms (best seen in inferior leads).
Image 3. Junctional bradycardia continues for 2 beats, followed by a sinus beat, then the rhythm returns to AF.
The 7th beat is a wide complex premature beat with no preceding P-wave, and may be a PVC (arising from a ventricular focus) or an Ashman beat (an aberrantly conducted beat arising from a supraventricular focus).
Overall, these findings suggest sinus node dysfunction, also called sick sinus syndrome.
Case Resolution
Labs were unremarkable for any significant abnormalities. Shortly after this ECG was obtained, the monitor showed multiple 3- to 4-second pauses. The patient did not require external pacing and was admitted for placement of a permanent pacemaker.
LEARNING POINTS
Sinus node dysfunction (sick sinus syndrome) ECG findings:
- Inappropriate sinus bradycardia: persistent bradycardia unable to meet physiologic demands
- Sinoatrial exit block: depolarization fails to exit the sinus node resulting in a dropped P-QRS-T complex
- Sinus pause/arrest: depolarization fails to exit the sinus node resulting in a dropped P-QRS-T complex
- Tachycardia-bradycardia syndrome: alternating episodes of bradycardia and tachycardia (often PSVT)
Junctional bradycardia ECG findings:
- Regular narrow complex QRS in the absence of conduction abnormalities
- Rate <40 bpm
- May have retrograde P-waves before (with PR interval <120 ms) or after QRS
Atrial fibrillation vs. Atrial flutter:
- AFib: f-waves with varying morphologies, duration, and timing
- AFlutter: f-waves with a uniform morphology, duration, and timing with no isoelectric baseline in lead II



