Case.
A 71-year-old male presents with exertional syncope.
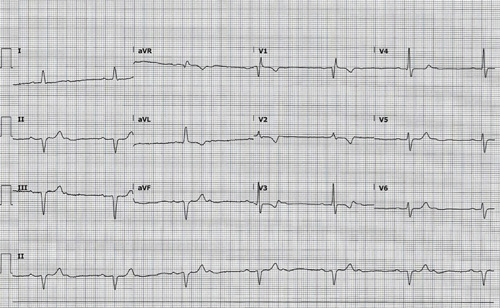
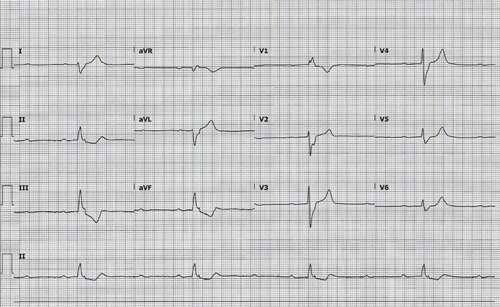
What do you see in the following ECGs (taken 4 minutes apart)?
Answer
Image 1. This ECG shows an atrial rate of ~78 bpm, a ventricular rate of ~39 bpm, and left axis deviation. There is a conduction block of every other beat, creating a repeating pattern of P-QRS-P with a constant PR interval for the conducted beats. This is a 2:1 AV block, which is an example of a fixed ratio AV block. Since every other beat is dropped in this ECG, it is impossible to determine if the PR interval is lengthening or not. This makes it difficult to tell if the underlying rhythm is a Mobitz Type I or Mobitz Type II. A wide QRS suggests a Mobitz Type II, but a narrow QRS, like the one seen in this ECG, can be seen with both Type I and Type II.
Image 2. This ECG shows a 3rd degree AV block, also called a complete heart block. The atrial rate is still ~78 bpm (note that every 3rd P-wave is buried in a T-wave) but the ventricular rate is now ~25 bpm. This ECG could easily be mistaken for a high-grade 3:1 AV block given how close the ventricular rate is to being 1/3rd of the atrial rate. But the PR intervals (for the conducted beats) are not constant- they are getting longer because the ventricular rate is little slower than 1/3rd of the atrial rate. Another difference to note is that the QRS is completely different in the 2nd ECG. It is now wide with rightward axis and there is a right bundle branch block. This suggests that ventricular is being paced infranodally, most likely from an idioventricular focus as there was no RBBB in the initial ECG. There are also T-wave inversions and ST depressions in the inferior leads of unknown etiology. The patient had no anginal symptoms and a negative troponin, which suggests these changes are repolarization abnormalities unrelated to ischemia.
Learning Points
2nd Degree AV Block: Mobitz Type I (Wenckebach)
General Features
- Intermittent failure of conduction, typically at AV node
EKG Features
- Relatively constant PP interval
- Progressively †‘PR interval and †“RR interval until a dropped QRS
- PR interval immediately after dropped beat is shorter than PR interval preceding dropped beat
- RR interval that includes blocked P-wave ‰¤ twice the PP interval
Clinical Significance
- Can be normal variant
- Does not produce hemodynamic compromise
- Can lead to a more advanced AV block if associated with a pathologic etiology
- Can be seen with inferior MI
2nd Degree AV Block: Mobitz Type II
General Features
- Intermittent failure of conduction, typically infranodal (ie, in His-Purkinje system)
EKG Features
- Relatively constant PP interval
- Constant PR interval in conducted beats
- Described as ratio of P-waves to QRS complexes
- QRS duration depends on location of block
— Narrow QRS ‡’ block in AV node or bundle of His
— Wide QRS ‡’ block distal to bundle of His - RR interval that includes blocked P-wave = twice the PP interval
Clinical Significance
- Always pathologic, never normal variant
- Frequently produces hemodynamic compromise
- Atropine is unlikely to lead to clinical improvement
- High risk of progression to 3rd degree AV block
- High-grade (or advanced) AV block
— Variant of Mobitz Type II where ‰¥ 2 sequential P-waves are not conducted
— Seen with anterior MI and has significant risk of progression to 3rd degree AV block
2:1 AV Block
General Features
- Conduction block of every other beat
EKG Features
- Every other QRS is dropped
- Wide QRS suggests underlying Mobitz Type II
Clinical Significance
- Not always possible to tell if the underlying block is Mobitz Type I or Type II so assume the higher risk Type II physiology
3rd Degree AV Block
General Features
- Absence of conduction through the AV node leading to complete AV dissociation
EKG Features
- P-waves “march out” (constant PP interval) and do not conduct to produce a QRS
- Regular PP interval that is shorter and independent of regular RR interval
- Atrial rate > ventricular rate
- Ventricular rhythm can be junctional (narrow QRS) or idioventricular (wide QRS)
Clinical Significance
- All patients require admission and evaluation for pacemaker placement
- Can be seen with inferior and/or anterior MI



