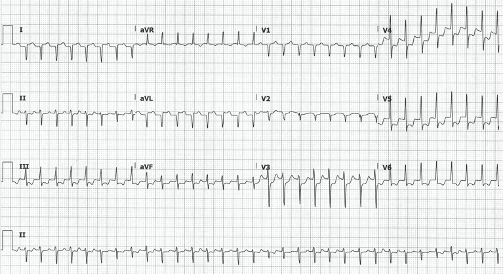
A 46-year-old male with a history of hypertension presents with palpitations and lightheadedness. What is your interpretation of the ECG?
Answer
This ECG shows a regular narrow-complex tachycardia with a ventricular rate of 190 bpm, right axis deviation, STE in leads I and aVL, and STD in II, III, aVF, and V2-V6.
The differential for a regular narrow-complex tachycardia includes:
- Atrial Flutter
- Atrial Tachycardia
- AV Nodal Reentry Tachycardia (AVNRT)
- AV Reentry Tachycardia (AVRT) with orthodromic conduction
- Junctional Tachycardia
The absence of discernible P-waves rules out sinus tachycardia and atrial tachycardia. The difference between these two is the morphology of the P-waves. Atrial tachycardia, which originates from a single ectopic focus in the atrium and is associated with structural heart disease,1 produces P-waves that are morphologically different compared to sinus rhythm.1
Junctional tachycardia, which is associated with ventricular rates of 90-140 bpm, is unlikely given the rate of 196 bpm seen in this EKG.
Atrial flutter with 2:1 conduction should be considered in any regular NCT with ventricular rates between 125-175 bpm.1 Flutter waves typically have a fixed rate of 250-350 bpm with a uniform morphology and are best seen in leads II and V1. Note that the classic saw-tooth pattern is not always obvious with 2:1 conduction.1
AVRT is reentry tachycardia that involves the AV node and an accessory pathway (eg, the Bundle of Kent in patients with WPW). Conduction down the AV node and back up the AP is called orthodromic conduction and will result in a NCT that mimics AVNRT. Conduction down the AP and back up the AV node is called antidromic conduction and will result in a WCT that mimics VT.
AVNRT is a reentry tachycardia that involves two pathways in or around the AV node. It is a common cause of paroxysmal SVT that is typically seen in young patients with no structural heart disease.1 It is triggered by a PAC that conducts down the slow pathway of the AV node while the fast pathway is still refractory from the previous impulse. By the time the impulse reaches the His-bundle, the fast pathway is no longer refractory, and this allows the impulse to simultaneously conduct anterograde to the ventricles and retrograde to the atria via the fast pathway.1 This circuit will continue until it is terminated by another PAC or with medical intervention (eg, vagal maneuvers, etc.). The retrograde conduction to the atria leads to retrograde P-waves which will point in the opposite direction of those seen in normal sinus rhythm on a baseline ECG.
This EKG also shows RA-LA lead reversal. An easy way to scan for lead reversal is to compare leads I and V6 which should look similar since they both look at the heart from the same direction. In this case, lead I points down and V6 points up which suggests that lead I's "view" is coming from the opposite side of the body. This is consistent with reversal of the arm leads. Another clue is that the QRS in aVR is predominantly upright. This is very atypical outside of dextrocardia in which case there would also be dominant S-waves in all of the precordial leads.4 If you mentally invert lead I and swap leads aVR and aVL, this ECG actually shows STE in aVR with diffuse STD. This pattern is seen in both ACS5 and non-ACS6 presentations. Tachydysrhythmias are a common non-ACS cause and is the likely etiology in this case.
Case Conclusion
This patient was successfully cardioverted to NSR with adenosine after vagal maneuvers were unsuccessful. Note that if this patient were in 2:1 flutter, treatment with an AV nodal blocker would have resulted in flutter waves with no QRS complexes, so treatment with adenosine was both therapeutic and diagnostic. A repeat ECG with correct lead placement showed a normal axis and no STE or STD. The remainder of the patient’s workup was unremarkable and he was discharged with cardiology follow-up.
AVNRT Learning Points
General Features:
- Also called PSVT
- Re-entrant circuit within or around the AV Node, typically triggered by a PAC
EKG Features:
- Rate typically 140-280 bpm
- Retrograde P-waves can appear before, after, or superimposed on QRS
- P-waves after QRS- appear as a pseudo S-wave in inferior leads and a pseudo R-wave in V1
- P-waves before QRS: very rare and morphology doesn't meet sinus criteria
LA-RA Lead Reversal Learning Points
|
I |
II |
III |
aVR |
aVL |
aVF |
V1-V6 |
|
Inverted |
Switches with III |
Switches with II |
Switches with aVL |
Switches with aVR |
No change |
No change |
For more information, please refer to pages 20-22 and 72 in the EMRA EKG Guide.
References
- Goldberger Z, Baman T. (2014). Inpatient Cardiovascular Medicine. John Wiley and Sons, Inc.
- Batchvarov V, Malik M, Camm A. (2007). Incorrect electrode cable connection during electrocardiographic recording. EP Europace, 9(11), 1081-1090. https://academic.oup.com/europace/article/9/11/1081/479121.
- Burns E. (2019, April 28). ECG Limb Lead Reversal. Life in the Fast Lane. https://litfl.com/ecg-limb-lead-reversal-ecg-library/
- Nickson C. (2019, July 3). Dextrocardia. Life in the Fast Lane. https://litfl.com/dextrocardia-ecg-library/
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definitions of MI. Journal of the American College of Cardiology. 2018;72(3), 2231-2264. https://www-sciencedirect-com.ezproxy.cul.columbia.edu/science/article/pii/S0735109718369419?via%3Dihub. Accessed March 23, 2020.
- Harhash AA, Huang JJ, Reddy, S., et al. aVR ST Segment Elevation: Acute STEMI or Not? Incidence of an Acute Coronary Occlusion. The American Journal of Medicine. 2019;132(5), 622-630. https://www-sciencedirect-com.ezproxy.cul.columbia.edu/science/article/pii/S000293431930049X?via%3Dihub#!. Accessed March 23, 2020.



