A 62-year-old female presents with 1 hour of crushing substernal chest pain. What is your interpretation of this EKG?
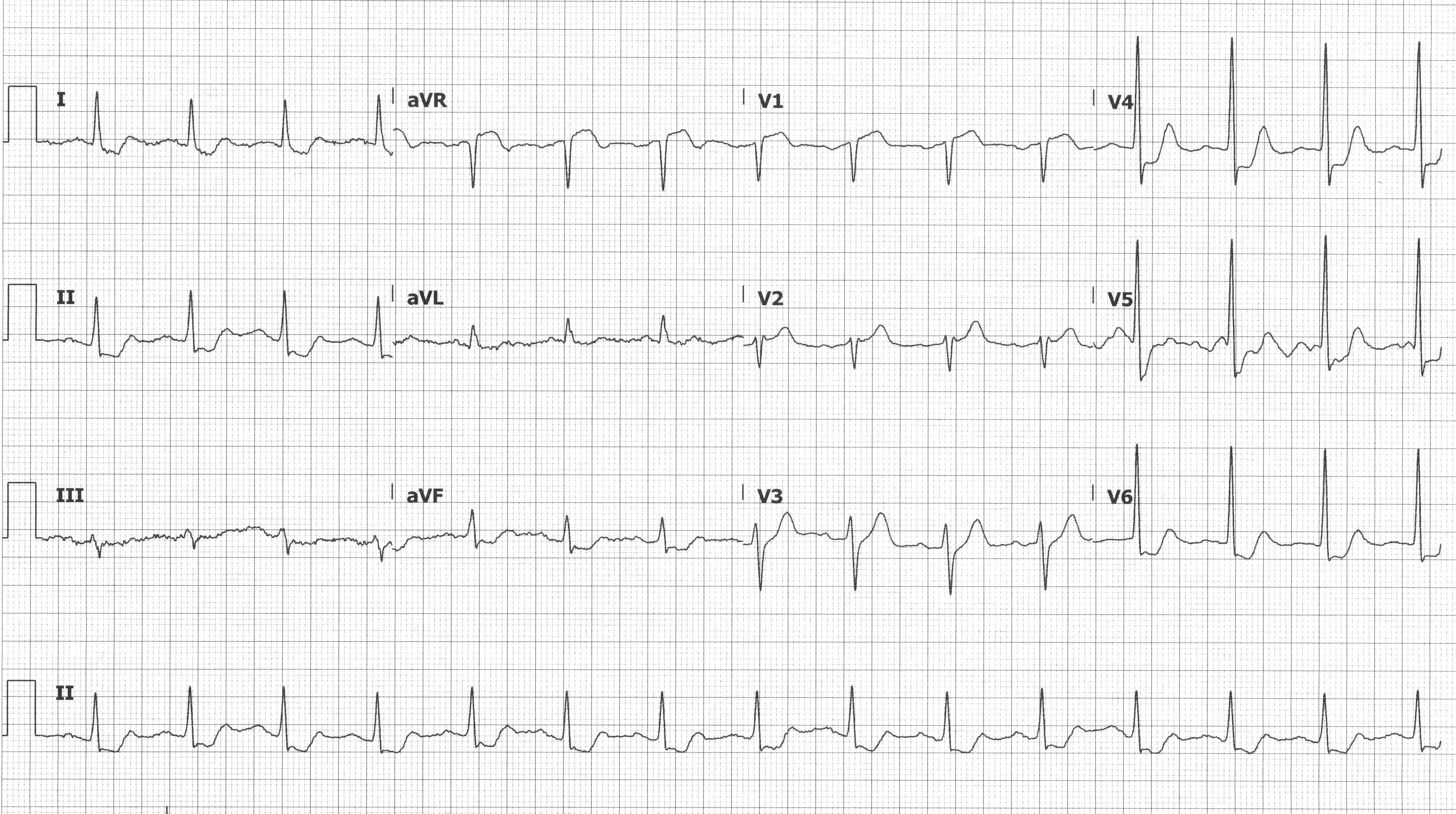
STE in aVR
This ECG shows a normal sinus rhythm with a ventricular rate ~90 bpm, STE in aVR and V1, and STD in leads I, II, aVF, V3-V6 (and possibly III, but it's hard to tell because of the baseline artifact). The pattern of STE in aVR +/- V1 with diffuse STD is seen in both ACS and non-ACS presentations. In ACS presentations, it can represent left main coronary artery insufficiency (commonly with STE aVR > V1), proximal LAD insufficiency (commonly with STE V1 > aVR), or triple vessel disease.1 While STE in aVR with diffuse STD does not meet "traditional" STEMI criteria, the 2013 ACCF/AHA Guidelines for the Management of STEMI recommend invasive angiography for patients with this ECG pattern and a presentation concerning for ACS.2
Since we treat patients and not ECGs, it is important to recognize the non-ACS etiologies of this ECG pattern. Consider the following ECG from a 65-year-old female presenting with chest pressure and shortness of breath.
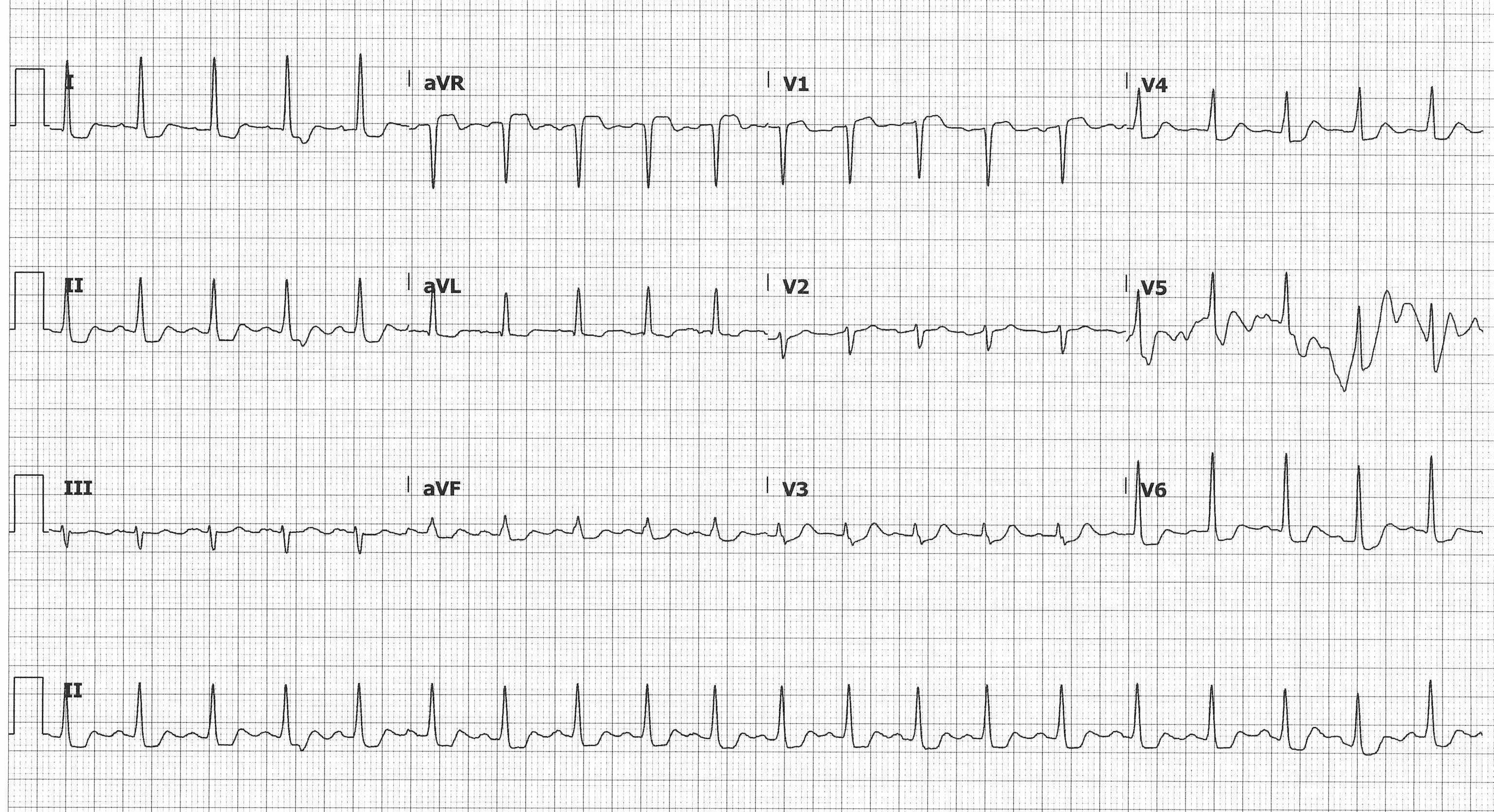
The patient was noted to be hypoxic to 85%, which corrected with supplemental oxygen. Initial CXR showed pulmonary edema and subsequent CTA was negative for PE. Labs were notable for a hemoglobin of 6.0, down from 12.2 a week prior. In this case, the patient's severe acute onset anemia led to subendocardial ischemia and decompensated heart failure, which led to pulmonary edema and hypoxia. The patient received a blood transfusion and judicious diuresis, correcting the underlying problem, after which her ECG normalized. Other non-ACS causes of STE in aVR include LVH with strain pattern, LBBB, aortic dissection, tachydysrhythmias, GI bleed/acute blood loss anemia, and pulmonary embolism. Accordingly, it is important to consider the non-ACS causes of this ECG pattern based on the patient's overall clinical picture.
aVR LEARNING POINTS
- aVR "looks at" the right upper portion of the heart including the basal part of the septum.
- STE in aVR with diffuse STD can result from ACS or non-ACS etiologies, so always consider the clinical context when going through the differential.
- ACS causes include proximal LAD or LMCA insufficiency or triple vessel disease.
- Does not meet "traditional" STEMI criteria, but the 2013 ACCF/AHA Guidelines for the Management of STEMI recommend invasive angiography for aVR LEARNING POINTS patients with this ECG pattern and a presentation concerning for ACS2
- Non-ACS causes include LVH with strain pattern, LBBB, aortic dissection, tachydysrhythmias, GI bleed/ acute blood loss anemia, and pulmonary embolism.
- ECG changes should resolve with resolution of non-ACS cause.
- Anterior or inferior AMIs with STE > 1 mm in aVR are associated with an increased 30-day mortality.3
Case Conclusion
The case was discussed with cardiology, and after the patient's symptoms resolved with medical management, she was admitted to the Cardiac ICU. Trended troponins were negative and cardiac catheterization the next morning showed a 90% ulcerated occlusion of the mid-LAD and non-obstructive left circumflex and RCA disease. The LAD occlusion was treated with a single drug eluting stent and the patient was discharged to cardiac rehab after an uneventful recovery.
For more details, please see pages 1 and 67 of the EMRA EKG Guide.
References
1. Thygesen K, Alpert JS, Jaffe AS, et al., on behalf of the Joint ESC/ACC/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction. J Am Coll Cardiol. 2018;8:1038.
2. O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2012;127:529-555.
3. Wong CK, Gao W, Stewart RA, et al. aVR ST elevation: an important but neglected sign in ST elevation acute myocardial infarction. Eur Heart J. 2010;31(15):1845–1853.



