Case
An 89-year-old male with history of coronary artery disease, ESRD, diabetes mellitus, and dual chamber permanent pacemaker placement presents with chest pain. What is your interpretation of his ECG?
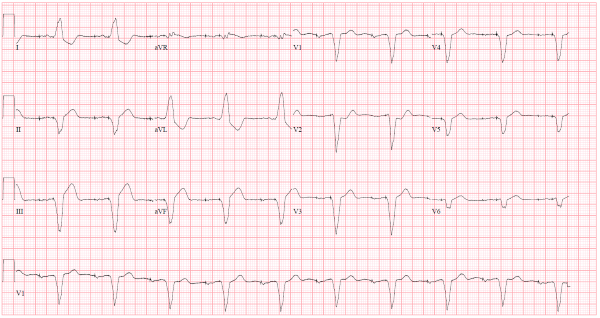
Image courtesy of Logan Weygandt, MD, MPH, Associate Program Director, Emergency Medicine Residency, and Edana Mann, MD, Johns Hopkins Hospital
Answer
This ECG shows a dual-chamber paced rhythm at 60 bpm, left axis deviation, prolonged QRS complex duration with left bundle-branch block-like morphology, STE in leads II, III, and aVF, and STD in leads I, aVL, and V2. The STD in lead V2 is diagnostic of an acute myocardial infarction (AMI).
Dual-chamber pacing, also called A-V sequential pacing, involves pacing of both the right atria and right ventricle. There is one atrial lead in the right atrial appendage and one ventricular lead in the right ventricular apex. The ECG will show 2 pacer spikes: one preceding the P wave and one preceding the QRS complex. The major difference in the QRS complex morphology between an intrinsic LBBB and a right ventricular-paced rhythm is that the QRS complex will almost always be negatively oriented in leads V5-V6 with a right ventricular-paced rhythm.
As with an intrinsic LBBB, the expected repolarization abnormalities in an RV paced rhythm follow the “rule of appropriate discordance” which describes the relationship between the direction of the QRS complex and its ST-segment. In other words, if the main vector of the QRS complex points up, there will be STD, and if the QRS complex points down, there will STE. These repolarization abnormalities confound the ECG’s ability to detect an AMI and other ACS findings, so interpretation of the ECG in a presentation suggestive of ACS requires using the Sgarbossa or Modified Sgarbossa criteria to diagnose an AMI.1
The Sgarbossa criteria are based on the underlying principle that concordance and excessive discordance in a LBBB or right ventricular-paced rhythm are abnormal. The modified Sgarbossa criteria (see Figures 1a-c) improve the sensitivity of the Sgarbossa criteria by defining excessive discordance as a ratio instead of a fixed number. Both criteria are included in the most recent AMI guidelines, but it makes sense to just use the modified Sgarbossa criteria since they are more sensitive than the traditional Sgarbossa criteria.
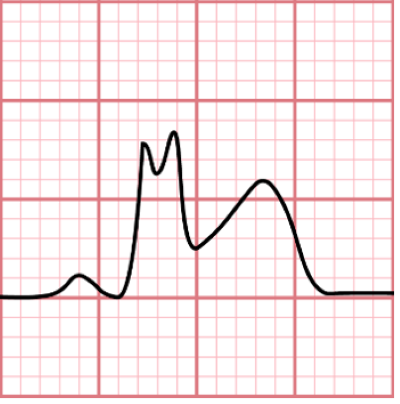
Figure 1a. Modified Sgarbossa criterion A: concordant STE ≥ 1 mm in ≥ 1 lead
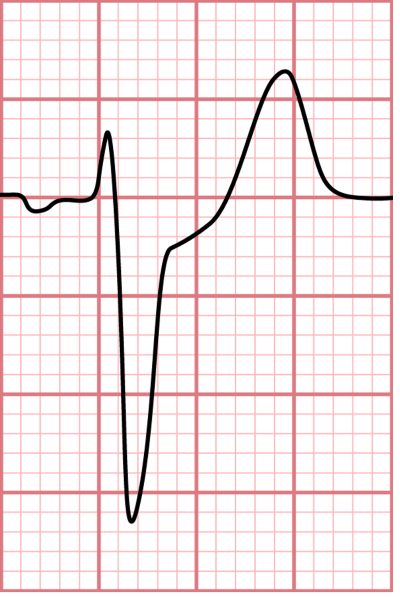
Figure 1b. Modified Sgarbossa criterion B: STD ≥ 1 mm in leads V1 or V2 or V3
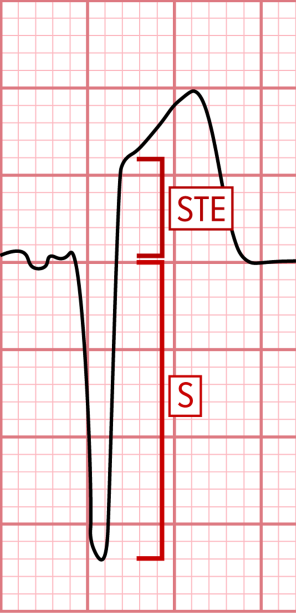
Figure 1c. Modified Sgarbossa criterion C: STE/S ratio ≥ 0.25 in ≥ 1 lead
Unlike traditional STEMI criteria that requires STE in 2 contiguous leads, the Modified Sgarbossa criteria only require changes in 1 lead. It is also important to note that a significant number of patients with AMI and a ventricular-paced rhythm will not have any abnormalities, Sgarbossa or otherwise, on their ECG.
In the case ECG, the STE in leads II, III, and aVF and the STD in leads I and aVL are appropriately discordant and do meet modified Sgarbossa criteria. The STD in lead V2 is concordant and meets modified Sgarbossa criterion B, which is diagnostic of an AMI.
Case Conclusion
This patient had multiple chronic conditions, which made him a poor candidate for cardiac catheterization, and his symptoms were well-controlled medically, so he chose to be admitted for continued medical management.
AMI in Right Ventricular-Paced Rhythms Learning Points
- Evaluate a right ventricular-paced rhythm for AMI as you would evaluate LBBB, using Sgarbossa or Modified Sgarbossa criteria1
- The presence of ≥ 1 of the following are diagnostic of AMI:
- Concordant STE ≥ 1 mm in ≥ 1 lead
- STD ≥1 mm in leads V1, V2, or V3
- Discordant STE ≥1 mm with a ratio of STE to S-wave depth ≥ 0.25 in ≥ 1 lead
- STD ≥1 mm in any of leads V4-V6 increases sensitivity for AMI2 but has not been externally validated at the time of this publication and is not included in the most recent 2022 ACC guidelines
References
- Kontos M, de Lemos J, et al. 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department. J Am Coll Cardiol. 2022;80(20):1925–1960.
- Dodd KW, Zvosec DL, Hart MA, et al. Electrocardiographic diagnosis of acute coronary occlusion myocardial infarction in ventricular paced rhythm using the modified Sgarbossa criteria. Ann Emerg Med. 2021;78:517–529.



