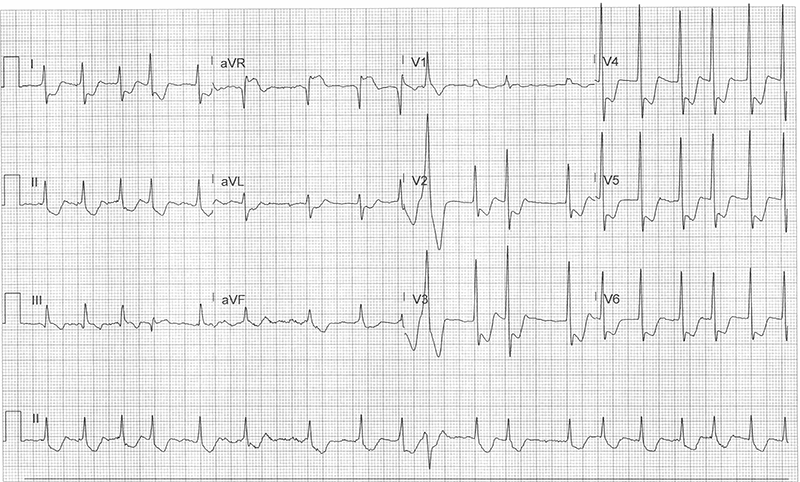
A 79-year-old male with a past medical history of coronary artery disease s/p CABG in 2012 presents with chest pain. His initial ECG showed atrial fibrillation with RVR at 168 bpm. Despite rate control with IV diltiazem, he continued to have chest pain. What is your interpretation of his ECG, obtained after giving diltiazem?
Answer
This ECG shows atrial fibrillation with an average ventricular rate of 110 bpm, normal axis, normal QRS complex duration, STE in lead aVR with STD in leads I, aVL, II, aVF, and V2-V6.
The differential diagnosis for the pattern of STE in lead aVR +/- lead V1 with diffuse STD includes both ACS and non-ACS etiologies. The patient’s initial ECG showed this pattern in the setting of much faster ventricular rates, so it would be reasonable to assume that the ECG changes were due to rate-related global cardiac ischemia. When considering non-ACS causes, it is expected that the ECG changes will resolve with treatment of the non-ACS cause. Given that the ECG changes persisted and the patient continued to have chest pain despite rate control, a non-rate-related etiology must be considered.
An important consideration for any ECG with STD in leads V1-V4, especially when seen with concurrent prominent R-waves and/or upright T-waves in these leads, is a posterior MI. Isolated posterior MI are easily missed as they do not show STE with the standard 12-lead placement.1 Posterior MI are typically seen with a concurrent inferior or lateral MI, but an estimated 5% of MIs are isolated posterior MI.
A repeat ECG with posterior leads (see Figure 1) was obtained and showed STE > 1 mm in lead V9 consistent with an isolated posterior MI. Note that the diagnostic criteria for a posterior MI only requires STE ≥ 0.5 mm (≥ 1 mm for men < 40 years old) in any one of the posterior leads (ie, STE in 2 contiguous leads is not required).
Figure 1. Repeat ECG with posterior leads V7-V9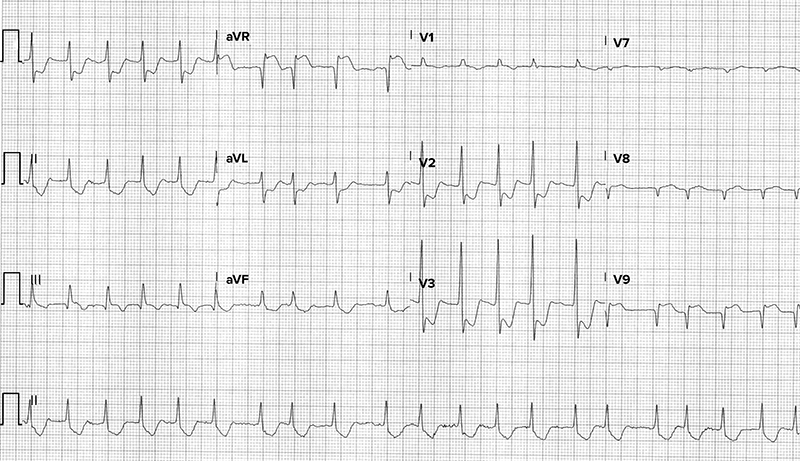
Conclusion
This patient was taken to the cardiac catheterization lab, where a 95% occlusion of the saphenous vein graft to the diagonal artery was successfully treated with a stent.
Lead aVR Learning Points
- STE in lead aVR +/- V1 with diffuse STD ≥ 1 mm in ≥ 6 leads can be due to ACS or non-ACS etiologies.
- In ACS presentations, this pattern is highly suggestive of LMCA obstruction, proximal LAD obstruction, and triple vessel disease, and immediate angiography should be considered.2
- In non-ACS causes, the ECG changes should resolve with treatment of non-ACS cause.
- Knotts et al. studied 113 patients with STE in lead aVR with diffuse STD, and of the 44% who underwent coronary angiography, only 23% were found to have left main (or equivalent) coronary artery disease.3
Always consider the clinical context when working through the differential diagnosis for this ECG pattern.
Posterior MI Learning Points
- Consider whenever there is STD in leads V1-V4, especially if there are concurrent prominent R-waves and/or upright T-waves in these leads.4,5,6
- The use of posterior leads is recommended but not mandated for the diagnosis of an isolated posterior MI, so local practice patterns typically dictate whether a posterior ECG is required for activation of the cardiac catheterization lab.
- Use posterior leads V7-V9 to evaluate for an isolated posterior MI if there is diagnostic uncertainty regarding STD in leads V1-V4.
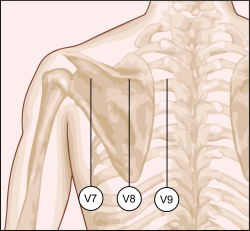
- V7: left posterior axillary line at the 5th intercostal space
- V8: left midscapular line at the 5th intercostal space
- V9: left paraspinal border at the 5th intercostal space
- STE ≥ 0.5 mm (≥ 1 mm for men < 40 years old) in posterior leads V7, V8, or V9 is diagnostic.
- Diagnosis does not require 2 contiguous leads.
References
- Levis JT. ECG Diagnosis: Isolated Posterior Wall Myocardial Infarction. Perm J. 2015 Fall; 19(4)e143-144. http://dx.doi.org/10.7812/TPP/14-244
- O’Gara PT, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. Circulation. 2013;127(4):e362-e425. DOI: 10.1056/NEJMc0804737
- Knotts RJ, et al. Diffuse ST depression with ST elevation in aVR: Is this pattern specific for global ischemia due to left main coronary artery disease? Journal of Electrocardiology, 2013; 46(3): 240-248. DOI: 10.1016/j.jelectrocard.2012.12.016
- Vasaiwala SC, Schreiber R. Posterior Myocardial Infarction: unique diagnosis to an elusive problem. American Journal of Emergency Medicine. 2008;26(520):e5–520.e6. DOI: 10.1016/j.ajem.2007.08.030
- Melendez J, Jones DT, Salcedo JR. Usefulness of three additional electrocardiographic chest leads (V7, V8 and V9) in the diagnosis of acute myocardial infarction. Can Med Assoc J. 1978;119(7):745-748.
- Wong CK. Usefulness of leads V7, V8, and V9 ST elevation to diagnose isolated posterior myocardial infarction. IJ Card. 2011;146(3):467-469.



