A 53-year-old male with unknown past medical history presents by EMS after a syncopal episode, acute shortness of breath, chest pain, and altered mental status. His initial vital signs are notable for hypoxia and hypotension.
What is your interpretation of the following ECG?
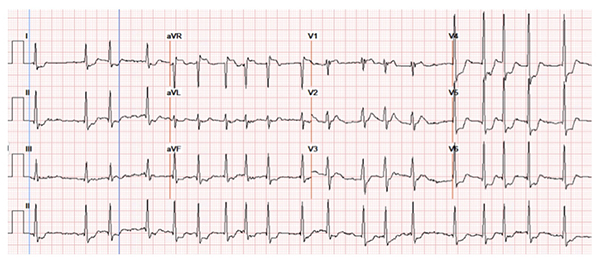
STE in aVR
The EKG shows atrial fibrillation with RVR at 115 bpm, ST elevations in aVR and V1, and ST depressions in I, aVL, II, aVF, V3, V4, V5, and V6. Unfortunately, there were no prior EKGs for comparison.
This pattern of STE in aVR and V1 with diffuse STD can be seen with the following: left main coronary artery (LMCA), proximal left anterior descending artery (LAD) insufficiency, diffuse subendocardial injury, and non-ACS causes such as right ventricular strain. It is important to determine the cause of this EKG pattern as emergent interventions may be indicated, such as PCI, CABG, or thrombolytics. Given the patient’s hypotension and hypoxia, the differential included ischemia of the inferior, anterolateral, basal septum regions or massive pulmonary embolism (PE) causing right heart strain.
While PE was strongly considered based on the patient’s history and vital signs, there are EKG features that argue for and against this diagnosis. Findings that could indicate RV strain or infarct include STE in V1 which is a rightward facing lead and the only standard EKG lead that is a direct reflection of the right ventricle. Additionally, STE in aVR, RBBB, and atrial fibrillation could all be explained by right-sided pressure overload. However, findings arguing against RV strain include a normal axis, neither significant STE or STD in lead III (which is the most rightward facing lead other than aVR), STE in aVR > V1, and lack of more pronounced ST-T wave changes in the anterior leads.
Learning Points
ST Elevation in aVR
General Features
- STE > 1 mm (0.1 mV) in aVR +/- V1, typically accompanied by diffuse STD
EKG Features
- aVR is most electrically opposite from II and V5
- Views the right upper heart, including the RV outflow tract and basal septum1
Clinical Significance
- Can be seen with triple vessel disease or insufficiency of the LAD or LMCA1,7
- STE in aVR > V1 suggests LMCA insufficiency, and higher STE predicts higher mortality2,7
- Widespread inferolateral STD with STE in aVR can be seen with acute occlusion of the LAD or LMCA, and can be considered a “STEMI Equivalent” in the right clinical scenario7
- STE > 0.05 mV in aVR has sensitivity of 68-91% and specificity of 73-80% for LMCA involvement6
- STE in aVR > 0.1 mV is associated with an in-hospital death rate of 19.4% compared to 1.3% without elevation in this lead (odds ratio = 6.6)5
- STE in aVR can be observed in patients with right heart strain secondary to acute PE
- STE in aVR can be a poor prognostic indicator in PE and more often presents with systolic blood pressure < 90 mmHg (27% vs 10%, p < 0.001)8
- In one study, 33.3% of patients with STE in aVR vs. 13.1% of those without died during hospitalization. In regard to hospital mortality, STE aVR had a low sensitivity of 25.8%, but high specificity of 90.5%.9
- STE in aVR can also indicate diffuse subendocardial ischemia, as O2 supply is not meeting demand. Other non-ACS causes include severe anemia, GI hemorrhage, or thoracic aortic dissection.
- Other instances where AVR may be helpful:7
- Posterior wall STEMI in patients with severe multivessel coronary artery disease
- Limb lead reversal – as seen by reversal of P-waves, QRS, T-waves in I and aVR
- Pericarditis
- Tall R-wave in aVR can suggest sodium channel blocker poisoning
- Help differentiate AVNRT from AVRT
- Detecting inverted P-waves and AV-dissociation in aVR confirming the diagnosis of ventricular tachycardia
Case Conclusion
Cardiology was emergently consulted for possible STEMI. Based on bedside US that showed enlarged RV and dilated IVC, the cardiology team felt that right heart strain and endocardial injury were driving the EKG findings and recommended a CT PE study, which showed bilateral large PEs. The STD were likely due to LV subendocardial injury from hypoxemia and hypotension, the STE in aVR and V1 from RV transmural ischemia from the outflow tract obstruction, and the isoelectric ST segment in lead III from the summation of the STE and STD. tPA was administered after which the patient’s hypotension, hypoxia, and altered mental status all resolved. He was admitted to the Medical ICU and subsequent formal TTE showed normal LV function. He was discharged 4 days later.
Final Diagnosis: Acute Saddle Pulmonary Embolism
References
1. Gorgels AP, Engelen DJ, Wellens HJ. Lead aVR, a mostly ignored but very valuable lead in clinical electrocardiography. J Am Coll Cardiol. 2001;38(5):1355-1356.
2. Yamaji H, Iwasaki K, Kusachi S, et al. Prediction of acute left main coronary artery obstruction by 12-lead electrocardiography: ST segment elevation in lead aVR with less ST segment elevation in lead V1. J Am Coll Cardiol. 2001;38:1348–1354.
3. Kireyev D, Arkhipov MV, Zador ST, Paris JA, Boden WE. Clinical utility of aVR-The neglected electrocardiographic lead. Ann Noninvasive Electrocardiol. 2010;15(2):175-180.
4. Rebel EM. REBEL Cast Episode 23: Is ST-Segment Elevation in Lead aVR Getting Too Much Respect? with Amal Mattu. https://rebelem.com/is-st-segment-elevation-in-lead-avr-getting-too-much-respect-with-amal-mattu/. Accessed May 20, 2019.
5. Barrabés JA, Figueras J, Moure C, Cortadellas J, Soler-Soler J. Prognostic value of lead aVR in patients with a first non-ST segment elevation acute myocardial infarction. Circulation. 2003;108:814-819.
6. Kosuge M, Ebina T, Hibi K, et al. An early and simple predictor of severe left main and/or three-vessel disease in patients with non-ST-segment elevation acute coronary syndrome. Am J Cardiol. 2011;107(4):495-500.
7. Lowenstein, SR. Critical Cases in Electrocardiography: An Annotated Atlas of Don't-Miss ECGs for Emergency Medicine and Critical Care. 1st ed. Cambridge, United Kingdom: Cambridge University Press; 2018.
8. Kukla P, Dlugopolski R, Krupa E, et al. The prognostic value of ST-segment elevation in the lead aVR in patients with acute pulmonary embolism. Kardiol Pol. 2011;69(7):649–654.
9. Pourafkari L, Ghaffari S, Tajlil A, Akbarzadeh F, Jamali F, Nader ND. Clinical Significance of ST Elevation in Lead aVR in Acute Pulmonary Embolism. Ann Noninvasive Electrocardiol. 2017;22(2).



