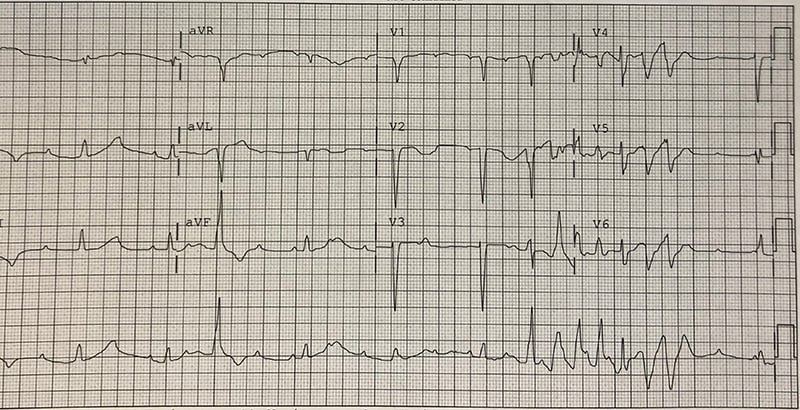
A 24-year-old male with history of intravenous drug use and tricuspid valve replacement 10 days ago presents with pain at his sternotomy site. The surgery was performed at another hospital, and the patient left there against medical advice yesterday. What is your interpretation of his EKG?
Answer
This EKG shows a 3rd degree AV block with a junctional escape rhythm at a rate of 55 bpm, right axis deviation, prolonged QTc interval, intermittent PVCs, and a non-sustained run of an irregular wide-complex tachycardia consistent with torsades de pointes (ie, polymorphic ventricular tachycardia in the presence of prolonged QTc).
Polymorphic ventricular tachycardia (PMVT) is a form of ventricular tachycardia resulting from multiple ventricular foci causing QRS complexes with varying morphology. EKG findings include an irregular wide-complex tachycardia with beat-to-beat variation in the QRS complex morphology and/or axis. It is called torsades de pointes (TdP) if there is a prolonged QTc interval on a baseline EKG; otherwise, it is classified as non-torsades PMVT. The etiology of TdP is a prolonged QTc interval, which can be either congenital or acquired. It is typically paroxysmal and self-terminating but can degenerate into ventricular fibrillation. Non-torsades PMVT is most commonly caused by myocardial ischemia. It is often constant and frequently leads to hemodynamic compromise.
Treatment of PMVT includes defibrillation for unstable patients regardless of etiology. For intermittent TdP, initial treatment includes IV magnesium sulfate. Electrical overdrive pacing can also be used, since increasing the ventricular rate leads to a decreased QTc interval, which lowers the risk of TdP recurring. Chemical overdrive pacing with isoproterenol should be avoided in patients with congenital long QT syndrome but can be used in patients with an acquired long QTc interval. Note that the paroxysmal nature of TdP makes direct cardioversion ineffective in preventing recurrence. For non-torsades PMVT, treatment is per ACLS protocol. All patients with polymorphic ventricular tachycardia should be seen by cardiology and admitted for further evaluation.
A 3rd degree AV block, also called a complete heart block and 3rd degree heart block, results from absence of conduction through the AV node. This leads to the atria and ventricles functioning independently of each other, which is called AV dissociation. Both the P-waves and R-waves should march out at regular rates with the atrial rate faster than the ventricular rate. Pacing of the ventricles occurs from below the AV node. If the pacing originates from the junction, the QRS complex will be narrow in the absence of a concurrent conduction abnormality (eg, preexisting bundle branch block). If the pacing is originating from the ventricle, the QRS complex will be wide. Common causes include ischemia, hypothyroidism, hyperkalemia, medications, and structural heart disease. Treatment is per ACLS protocol and all patients will require admission for evaluation for a pacemaker.
Case Conclusion
After obtaining this EKG, the crash cart was brought to the bedside and pads were placed on the patient. Treatment of the intermittent TdP was initiated with 2 g of IV magnesium sulfate, and cardiology was paged to evaluate for emergent transvenous pacemaker placement. Further inpatient workup after admission to the cardiac ICU was notable for an aortic root abscess in close proximity to the AV conduction pathway. EKGs obtained later throughout admission showed a QTc of 435 msec, suggesting a non-torsades etiology; the PMVT was likely secondary myocardial ischemia, as TTE showed reduced RV systolic function and high sensitivity troponin I was elevated at 88 (normal <20). The patient ultimately required a permanent pacemaker for a persistent 3rd degree AV block thought to be caused by the aortic root abscess and/or a complication from the tricuspid valve replacement.
PMVT Learning Points
- Wide complex ventricular rhythm >100 bpm with beat-to-beat variation in QRS axis and/or morphology
- Classified as either torsades or non-torsades
- Torsades de pointes
- Prolonged QTc interval (either congenital or acquired) on baseline EKG
- Characteristic twisting of the peaks of the QRS around the isoelectric baseline
- Usually paroxysmal and self-terminating but can degenerate into ventricular fibrillation
- Non-torsades
- Absence of QT prolongation on baseline EKG
- Often due to ischemia
- Usually sustained and causes hemodynamic instability
- Treatment
- Defibrillation for unstable PMVT regardless of etiology
- ACS workup for all non-torsades PMVT
- Identify and correct underlying cause(s) for non-torsades PMVT (eg, QT prolonging medications, hypokalemia, hypomagnesemia, hypocalcemia, elevated ICP, etc.)
- Magnesium, electrical overdrive pacing, and electrolyte repletion (if indicated) for intermittent torsades due to congenital or acquired long QT syndrome
- Chemical overdrive pacing with isoproterenol for intermittent torsades due to acquired long QT syndrome
3rd Degree AV Block Learning Points
- A 3rd degree AV block, or complete heart block, is defined by the absence of conduction through the AV node leading to complete AV dissociation
- P-waves march out (constant PP interval) and do not conduct to produce a QRS complex
- PR intervals are variable
- Atrial rate > ventricular rate
- Ventricular rhythm is usually junctional or ventricular escape rhythm
- All patients require admission and evaluation for pacemaker placement



