Case. A 97-year-old female with a past medical history of congestive heart failure with an ejection fraction of 20%, hypertension, and chronic left bundle branch block presents to the emergency department with the chief complaint of nausea, shortness of breath, and epigastric abdominal pain for 1-day duration. The patient states that her symptoms had started gradually around 10:30 PM and continued to get worse until her presentation in the morning.
What are you concerned about?
ANSWER
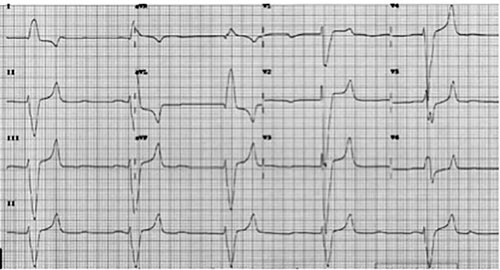
This ECG demonstrates a heart rate of 24 BPM, a left bundle branch block, and a QRS duration of 220ms. There are peaked T-waves with flat to widened P-waves intermittently, that do not necessarily associate with the QRS complexes. The ventricular rate with a widened QRS would suggest an idioventricular rhythm, giving us a complete third degree heart block with an idioventricular rhythm.
The patient had stopped taking her furosemide for the past week and continued taking her spironolactone. She was found to have a non-hemolyzed potassium of 9.6. The patient was hemodynamically stable from a blood pressure standpoint. However, had she become unstable, she would have undergone temporary pacing. While the patient was being prepared for dialysis, she received 1gm calcium gluconate, 20 units of regular insulin IV, 2 amps of D50, and a 10mg albuterol nebulizer treatment. Repeat potassium prior to starting dialysis was 8.0. Status post Quinton catheter placement, she underwent emergent dialysis. Repeat potassium post-dialysis was 6.2. Repeat 12-lead ECG showed normal sinus rhythm at 90 beats per minute with a decreased QRS diameter from 220 to 180. The patient remained hemodynamically stable and was transferred to the ICU for closer monitoring.
Our patient had a critically elevated potassium with an impending sine wave appearance and impending cardiac arrest. Emergent treatment was necessary to save the patient’s life.
Learning Points
- When a patient is noted to be bradycardic, especially if irregular, the clinician must always think of hyperkalemia.
- Hyperkalemia is the great masquerader, and ECG changes can be marked and varied.
- Hyperkalemia is one of the few potentially lethal electrolyte abnormalities that mandates prompt suspicion and recognition.



