International medical electives are becoming increasingly popular among EM residents as programs take the initiative to provide a valuable educational experience for their residents while ensuring time abroad provides value to the host institution.
Given the short-term nature of medical electives, this goal can prove rather challenging and usually requires the development of long-term relationships with host institutions. In this vein, the Palmetto Health/University of South Carolina Department of Emergency Medicine has sought to build sustainable impact through established long-term relationships with physicians at local medical centers in both Uganda and Tanzania.
Masindi-Kitara Medical Center
In Uganda, we have an ongoing collaboration with Masindi-Kitara Medical Center (MKMC) and the nonprofit organization OneWorld Health. Over the past 5 years, Palmetto Health faculty, residents, and alumni have traveled to Uganda several times per year to participate in outreach clinics, provide specialized training to hospital staff, and collaborate with local providers on research initiatives.
Physicians at MKMC have identified a need for trauma and critical care training among their hospital staff and other providers in the Masindi region. In response, our global health fellow and sub-specialty track resident have developed a unique, context-appropriate curriculum that utilizes both didactic lectures and simulations.
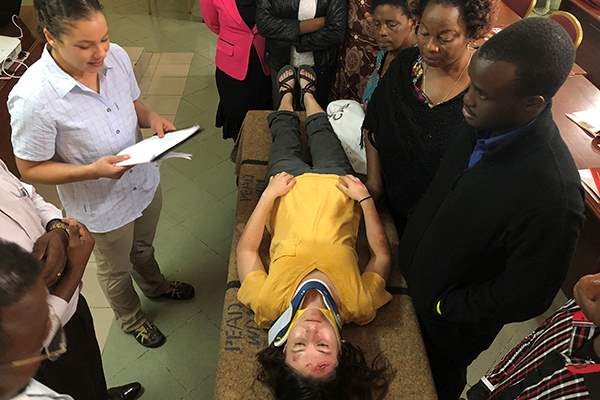
Although not a novel approach in the U.S., simulation medicine is truly a foreign concept for many of the providers we have encountered. In 2017, a multidisciplinary trauma training was implemented over 2 days in Masindi, which was attended by 40+ local and regional health care providers. This training utilized simulation supplies and standardized patients to replicate clinical scenarios and was the first training of its kind in the Masindi region.
We worked with our hospital’s simulation center to craft simple and affordable skills stations, and learned the art of moulage makeup to enhance the realism of each case. Although there were initial hurdles in conveying the concept of simulation, the course was very well-received and will become a recurring project.
The debut course focused on initial evaluation and stabilization of the critically ill patient. Materials addressed some of the area’s most common causes of illness. These lectures were supplemented by EM on-shift guides provided by EMRA.
In the simulations, participants worked together to recognize and stabilize critically ill patients with a variety of illnesses, including a ruptured ectopic pregnancy, a patient with cerebral malaria, and hypovolemic shock from cholera. Participants were able to practice needle decompression and chest tube placement on a novel, low-cost simulator, which the Palmetto Health Simulation Center helped us create.
By the end of the daylong course, participants were familiar with the concept of simulation and felt much more comfortable diagnosing and managing critically ill patients. We were able to train providers from 6 different hospitals, and the course was so successful that the local Minister of Health recognized our efforts.



Mbeya Zonal Referral Hospital
We then traveled to Mbeya Zonal Referral Hospital (MZRH) in Mbeya, Tanzania, where University of South Carolina (USC) family medicine, surgery, and EM departments have working relationships with local providers. We coordinated with a USC trauma surgeon and Mbeya’s only EM residency-trained physician to replicate trauma training.
Participants learned to manage blunt and penetrating trauma, burns, and orthopedic trauma. Their procedural and leadership skills were challenged when they were expected to “run” the trauma simulations as if they were in the ED setting. We had more than 70 participants over the course of 2 days, with overwhelmingly positive feedback.
Ongoing Collaboration
Over the course of 1 week, we traveled to 2 countries, trained 101 health care providers, gave 20 lectures, acted in 108 scenarios, and hopefully made a lasting impact on those communities. We believe this model provides an opportunity for impactful involvement for residents and faculty who are unable to spend several weeks abroad, but want to participate in a meaningful global health project. We hope to continue the relationships in Uganda and Tanzania.
The Ugandan collaboration continues with another multidisciplinary critical care conference, focusing on acute cardiac care, scheduled for spring. Presently in Tanzania, our global health EM program is continuing to partner with the USC surgery department and the Mbeya Zonal Referral center to introduce regional trauma training via simulation while simultaneously implementing the hospital’s first trauma registry.