Even with the introduction of selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCA) are still utilized in the treatment of major depressive disorders and chronic pain syndromes.10
Tricyclic antidepressants (TCA) inhibit presynaptic reuptake of norepinephrine and serotonin in the central nervous system (CNS). They are known to block different types of receptors such as peripheral alpha-adrenergic, histaminic, muscarinic, and central serotonin receptors which lead to various effects on the individual.11 Four pharmacological properties are primarily recognized for causing the toxic effects of TCAs: inhibition of norepinephrine reuptake at nerve terminals, direct alpha-adrenergic block, cardiac sodium and potassium channel blockade, and anticholinergic action.12 In comparison to an SSRI overdose, TCA overdoses are the cause of a higher rate of fatality and hospitalization in the United States.10 Doxepin is a tricyclic antidepressant that was primarily approved for depression but has also been approved by the Food and Drug Administration (FDA) to treat insomnia and anxiety.
Case
A 70-year-old male with a past medical history of major depressive disorder, gastritis, hypertension, atrial fibrillation, and recent cerebrovascular accident (CVA) with residual right eye peripheral vision loss was transported by emergency medical services (EMS) as he was unresponsive and had an altered mental status. Per EMS, there were two empty bottles of doxepin at the scene. Patient was recently released from the inpatient psychiatric facility after being admitted for reports of suicidal ideations. Patient had a laryngeal mask airway (LMA) placed by EMS at the scene, and the primary sources of history at the hospital were EMS and the patient's nephew.
In the ED, the patient was managed systematically with priority to airway, breathing and circulation. Initial vital signs were BP 135/60, HR 101, RR 18, and O2 saturation 100% on vent FiO2 100%. Patient’s GCS was 3 upon arrival at the ED. EKG showed normal sinus rhythm with QRS widening at 132 msec and QT interval at 434 msec.
Investigations
The initial EKG at arrival showed a normal sinus rhythm, ventricular rate of 96, QRS interval widening with duration 132 msec, and QTc interval widening at 548 msec. There is a nonspecific intraventricular conduction block present. When compared to a baseline EKG done one week ago, the ventricular rate had increased by 30, prolonged QRS and QT intervals.
Figure 1. Initial EKG
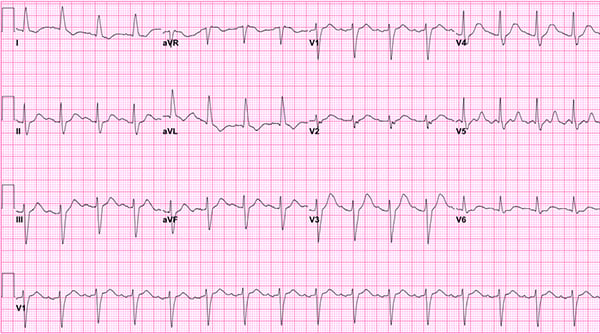
Figure 2. First repeat EKG
An EKG done 2 hours after arrival showed a normal sinus rhythm, ventricular rate of 87, prolonged QRS interval of 112 ms, and still prolonged QTc interval of 575 msec.
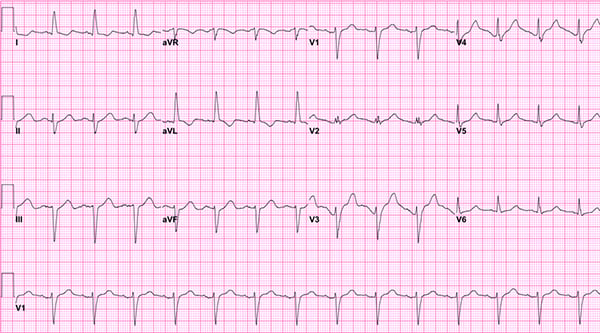
Figure 3. Second repeat EKG
EKG done 20 minutes later showed normal sinus rhythm, ventricular rate of 78, decreased QRS interval of 88 msec, and decreased QTc interval of 476 msec. There was no longer a nonspecific intraventricular conduction block.
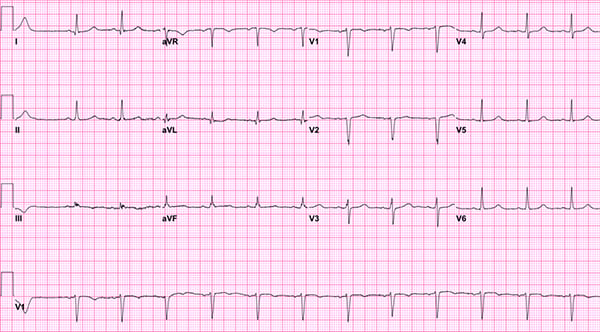
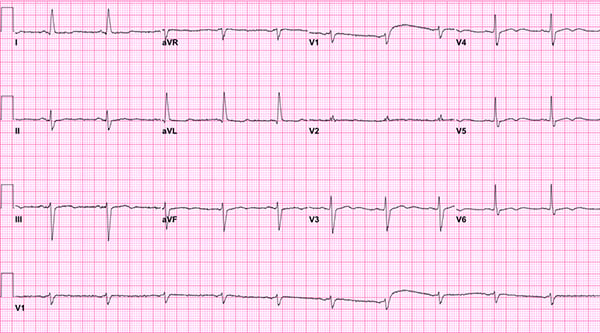
Figure 4. Next-day EKG
An EKG done the next day, about 24 hours after patient arrived to the emergency department, showed a normal sinus rhythm, ventricular rate of 63, QRS interval of 104 msec, and QTC interval of 462 msec. This EKG is similar to the one the patient had a week prior. All EKG abnormalities had resolved at this point.
Treatment
The patient’s airway, breathing and circulation were addressed once he arrived, and an EKG was ordered immediately. The patient had a LMA placed in the field for airway protection, and this was later replaced with a definitive endotracheal tube under video laryngoscopy. Patient was sedated with etomidate and paralyzed with rocuronium. Tube placement was confirmed, and the patient had bilateral breath sounds. Next, a triple lumen venous catheter was inserted in the right internal jugular vein for medication administration and fluid resuscitation. Given the patient's presentation and history concerning doxepin overdose, multiple steps were taken to prepare for management and treatment of the TCA overdose. During intubation, an Orogastric tube was placed, and the patient received 100g of activated charcoal. Sodium bicarbonate was ordered from the pharmacy, and a bicarbonate drip and norepinephrine were also ordered at bedside. For QRS >100msec, bolus was ordered at 1-2mEq/kg. This bolus can be repeated every 3-5 minutes until QRS <100msec. Infusion rate is 200cc/hr of 150mEq NaHCO3 in D5W. It’s recommended that these patient’s electrolytes and pH be monitored every 1 hour. Goal is to QRS that remains <100 msec and pH 7.45-7.55. QRS intervals should narrow within 60 seconds of sodium bicarb administration. Poison control was notified of the case, and they recommended treatment until the QRS interval became normal and to start a bicarbonate drip.
Outcome and Follow-Up
The patient was stabilized and transferred to the intensive care unit for further treatment and management. Patient was extubated the next day in the ICU and transferred to the floor for one day. The hospitalist team consulted psychiatry, and the patient was admitted to an inpatient psychiatric facility for suspected suicide attempt with doxepin.
Discussion
We present a case of suicide attempt by doxepin overdose in an elderly male patient with history of depression and recent CVA. Doxepin was first approved for use in the United States in 1969. The EKG is a highly utilized and important tool for emergency medicine physicians to diagnose many medical conditions including TCA overdose. There are many EKG abnormalities present with a TCA overdose.6 Some of the most common EKG findings for a TCA overdose include:
- Sinus tachycardia (most common EKG finding)
- Widening of the QRS greater than 100 msec
- Prolongation of the PR or QT interval
- Right bundle branch block
- Non-specific intraventricular conduction delay (IVCD)
- Wide-complex tachycardia
- Ventricular tachycardia/ventricular fibrillation
- Brugada pattern
QRS duration of >100msec increases the risk of seizures, and a QRS >160msec increases the likelihood of ventricular dysrhythmia.7 The QRS prolongation is not specific to TCA overdose but rather indicative of a sodium channel blockage.8 Other medications that block sodium channels include propranolol, carbamazepine, bupivacaine, and artiarrhythemics like quinidine, flecainide and procainamide.9
Another important aspect of this case is the history of both a CVA and depression. The relationship between stroke and depression has only recently been investigated, but it is estimated that depression affects about one-third of stroke survivors. Additionally, depression is also associated with poor functional outcomes for patients with recent stroke, poor quality of life, increased recurrent infarcts, and increased mortality.14 Currently, there insufficient guidance on the screening and treatment of depression in this high-risk population. Thus, future research on appropriate screening tools and interventions may reduce the rates of depression in this population.
In conclusion, our case highlights the EKG changes associated with doxepin overdose, particularly QRS widening and QT interval prolongation. We also demonstrated the systematic approach emergency physicians must take in caring for patients with doxepin overdose, which includes focus on airway, breathing and circulation followed by obtaining an EKG as soon as
possible. The treatment included sodium bicarbonate bolus followed by a sodium bicarbonate drip. Once the QRS interval had become normal, the patient was monitored in the ICU for 24 hours. Lastly, this case brings to light the need for improved mental health care in this country possibly to prevent similar cases in the future.
Disclaimer
This research was supported (in whole or part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this presentation represent those of the author and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Special Acknowledgement and thank you to Yash Patel MSII, Mercer University School of Medicine for his contribution.
References
- Rojas-Fernandez CH, Chen Y. Use of ultra-low-dose (≤6 mg) doxepin for treatment of insomnia in older people. Can Pharm J (Ott). 2014;147(5):281-289.
- Matheson E, Hainer BL. Insomnia: pharmacologic therapy. Am Fam Physician. 2017;96(1):29-35.
- Hawton K, Bergen H, Simkin S, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry. 2010;196(5):354-358. doi:10.1192/bjp.bp.109.070219
- Pinder RM, Brogden RN, Speight TM, Avery GS. Doxepin up-to-date: a review of its pharmacological properties and therapeutic efficacy with particular reference to depression. Drugs. 1977;13(3):161-218.
- Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Emerg Med J. 2001;18(4):236-241.
- Harrigan RA, Brady WJ. ECG abnormalities in tricyclic antidepressant ingestion. Am J Emerg Med. 1999;17(4):387-393.
- Niemann, JT, Bessen, H, Rothstein, R, and Laks, M. Electrocardiographic Criteria for Tricyclic Antidepressant Cardiotoxicity. Am J Cardiol. 1986; 57: 1154-1159.
- Mehta, n, and Alexandrou, N. Tricyclic Antidepressant Overdose and Electrocardiographic Changes. J of Emergency Medicine. 2000. 18(4): 463-464.
- Bruccoleri, RE, Burns, MM. A Literature Review of the Use of Sodium Bicarbonate for the Treatment of QRS Widening. J Med Toxicol 2016 Mar; 12(1):121-129.
- Clark S, Catt JW, Caffery T. Rapid diagnosis and treatment of severe tricyclic antidepressant toxicity. BMJ Case Rep. 2015 Oct 14;2015:bcr2015211428.
- Khalid MM, Waseem M. Tricyclic Antidepressant Toxicity. [Updated 2021 Feb 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430931/
- Kerr GW, McGuffie AC, Wilkie STricyclic antidepressant overdose: a reviewEmergency Medicine Journal 2001;18:236-241.
- Almasi A, Meza CE. Doxepin. [Updated 2021 May 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542306/
- Towfighi A, Ovbiagele B, El Husseini N, et al. Poststroke depression: a scientific statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2017;48(2).



