Dizziness is the third most common complaint reported in the ED. Asking the right questions and teasing out the details of this vague complaint can lead to proper management and reduced negative outcomes.
Dizziness is the third most common complaint reported in the ED, responsible for 5% of presentations to the ED and outpatient clinics, with a 30% lifetime prevalence. Asking the right questions and teasing out the details of this vague complaint can lead to proper management and reduced negative outcomes.
While there are many potential causes for dizziness, let’s look at how to differentiate between 4 common causes:
- Syncope
- Vertigo
- Disequilibrium
- Non-specific dizziness
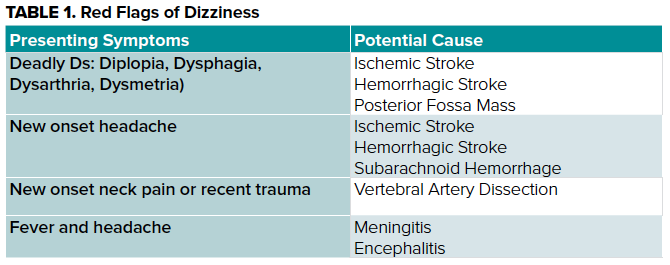
As a medical student, it can be difficult to determine which questions to ask to determine emergent, “can’t miss” (Table 1) vs. benign processes and how you will work up and potentially treat this patient, but the key to success all starts with a detailed history and physical exam.
Syncope/Near Syncope
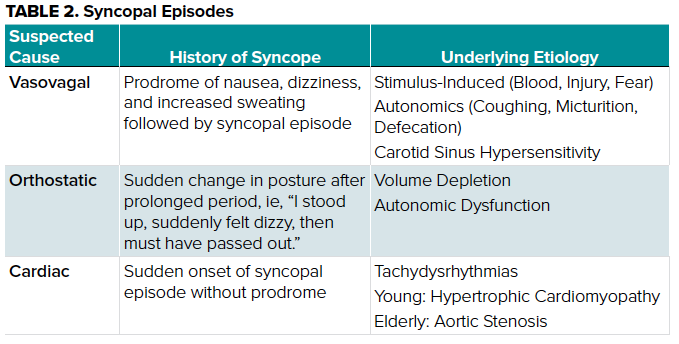
Syncope is defined as a transient loss of consciousness with accompanying loss of postural tone, followed by complete resolution and return to baseline. The syncopal patient will often describe a feeling of lost consciousness or blacking out. Determining syncope as a possible diagnosis for your patient requires appropriate questioning when eliciting a detailed history, capturing key data such as is noted in Table 2.
Vertigo
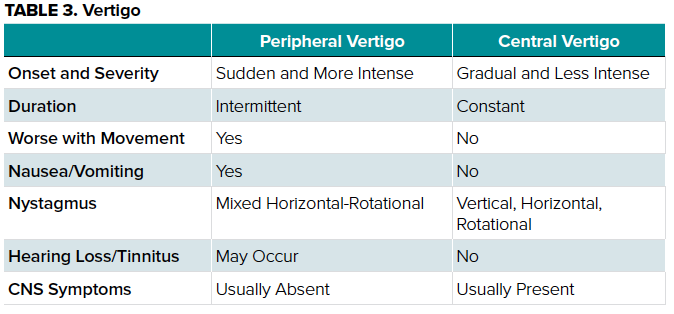
The patient with signs and symptoms of vertigo will classically present with the complaint of “the room is spinning,” due to mismatches in the perception of movement. The challenge in this diagnosis is identifying any potential “red flags” in the history and physical exam and differentiating between peripheral and central causes.
Medical students should be capable of discerning between the two with in-depth questions regarding onset, severity, and associated symptoms, as well as a detailed physical exam as described in Table 3.
HINTS
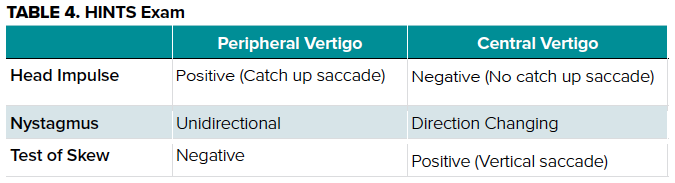
Additional physical examination testing in the form of the HINTS (Head Impulse, Nystagmus, Test-of-Skew) exam can distinguish between central and peripheral causes as described in Table 4.
Disequilibrium
Disequilibrium is characterized by a sense of imbalance with physical activity. The patient with suspected disequilibrium might describe a sensation they are “going to fall if I don’t have something to hold on to,” or “ I feel like I’m floating,” or even that “the world feels tilted.” These descriptors have been documented in the ED encounter for disequilibrium and can be your initial cue directing your H&P exam.
In most cases, these patients will present with past complaints of gait and/or visual disturbances leading to their sense of dizziness, which can then be attributed to significant past medical history of conditions such as peripheral neuropathy, musculoskeletal disorders, cerebellar disorders, and neurologic disorders.
Non-Specific Dizziness
This diagnosis should remain lower on your differential and only be utilized as a diagnosis of exclusion. Most patients are healthy and young without underlying comorbidities of the cardiovascular, pulmonary, or neurologic systems that could account for their symptoms. In a prospective study of 100 patients with chronic dizziness in ambulatory care conducted by Kroenke, et al, roughly 50% of the study population had a history of major epression/generalized anxiety/panic disorder, suggesting underlying psychiatric disorders as a potential cause of dizziness.
Conclusion
Dizziness is a common complaint and a challenge to the medical student during clerkships. Utilizing this approach can help you obtain a detailed history and physical exam, leading to a more appropriate differential diagnosis and treatment plan.
References
1. Branch W, Barton J. Approach to the patient with dizziness. UpToDate. June 2018.
2. Grimby A, Rosenhall U. Health-related quality of life and dizziness in old age. Gerontology. 1995;41:286-298.
3. Kroenke K, Lucas CA, Rosenberg ML, et al. Causes of persistent dizziness. A prospective study of 100 patients in ambulatory care. Ann Intern Med. 1992;117(11):898-904.
4. Mikhail MG. Syncope. In: Cline DM, Ma OJ, Cydulka RK, Meckler GD, Thomas SH, Handel D, eds. Tintinalli's Emergency Medicine Manual. 7th ed. New York City, NY: McGraw-Hill; 2012:131-134.



