The Patient
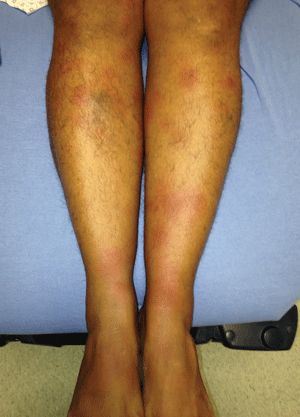
A 54-year-old female presents to the emergency department with a rash on her hands and legs that has progressed over the past day. She reports having used Lysol to clean the house yesterday and believes the rash started shortly after that. Further history reveals she started Bactrim 2 days ago for a back abscess, but the patient swears she has taken Bactrim in the past without any issues. The rash was initially erythematous and pruritic but progressed quickly. She now has blisters on the dorsum of her right hand and medial left wrist, and reports an associated tingling sensation. She denies fevers, chills, abdominal pain, nausea, vomiting, or diarrhea. Physical exam is unremarkable aside from the findings seen in the photographs.

What is the diagnosis?
Fixed Drug Eruption
This patient has a fixed drug eruption (FDE) likely secondary to Bactrim use. While many classes of drugs can cause FDEs, suspicion should be highest in patients who have a history of antibiotic, NSAID, anti-epileptic, sedative, or anti-malarial use. The rash typically presents as well-demarcated, round or oval red macules, but it can evolve into plaques or bullae. An associated tingling or burning sensation, as this patient described, is also common. The reaction can occur anywhere from 30 minutes to several days after exposure.
The diagnosis is usually clinical; however, histopathology may be helpful if atypical features are present. Treatment of FDEs in the acute setting involves symptomatic control in the form of systemic antihistamines and/or topical corticosteroids. The use of systemic corticosteroids is not well established. The lesions typically resolve spontaneously over the course of a week after cessation of the offending agent. FDEs can recur if there is subsequent exposure to the offending agent or to an agent with cross-reactivity. Thus, patch testing and oral provocation may be performed to identify the suspecting agent several weeks after the inciting event.



