Decompression Sickness (DCS) is a result of the formation of gas bubbles in body tissues during descent and subsequent re-circulation during depressurization or ascent. The majority of cases occur in divers.
Case
A 50-year-old male with no significant past medical history presents to the emergency department after a recreational dive to ninety feet one day prior. Upon surfacing, the patient developed confusion, bilateral shoulder pain, lower extremity weakness, and lower extremity paresthesias. After resurfacing, he was administered supplemental oxygen by his dive company for 2 hours, and his symptoms improved. The next day he developed recurrence of his bilateral shoulder pain and lower extremity paresthesias, prompting a visit to the ED.
On examination he was well-appearing with stable vital signs. He had full range of motion in all his extremities and strength was 5/5 and symmetric in both the upper and lower limbs. His tympanic membranes were intact bilaterally, pulses were equal and symmetric, and had no objective sensory deficit. The remainder of his physical examination was unremarkable. A complete blood count, comprehensive metabolic panel, and chest x-ray were unremarkable. The patient was given supplemental oxygen via a non-rebreather mask and started on IV fluids for suspected decompression sickness. The Diver's Alert Network (DAN) was consulted and recommended transfer for hyperbaric therapy.
Discussion
Decompression Sickness (DCS) is a result of the formation of gas bubbles in body tissues during descent and subsequent re-circulation during depressurization or ascent. The majority of cases occur in divers. Other populations affected are caisson (watertight chamber) workers, high-altitude pilots, and astronauts.1
The pathophysiology behind DCS requires an understanding of Henry's law, which states that at a constant pressure, the amount of gas dissolved in a liquid is directly proportional to the partial pressure of that gas. Take, for example, a diver: an individual descends in the water, ambient pressure increases by approximately one atmosphere every 33ft of depth in saltwater. When a diver takes a breath of compressed air in this increasingly pressurized environment, inert gases in the air (mostly nitrogen) have increased solubility in blood and begin to saturate the diver's tissues until a state of equilibrium is reached. During ascent, or decompression, ambient pressure decreases, and nitrogen is released from these tissues. The nitrogen gas eventually travels to the lungs, where it is released with exhalation ("off-gassing"). DCS occurs when overly rapid ascent leads to insufficient nitrogen washout by the lungs and the gas bubbles remain trapped in various tissues. This becomes clinically apparent when the liberated gas causes mechanical tissue compression and/or embolization to the venous system.2
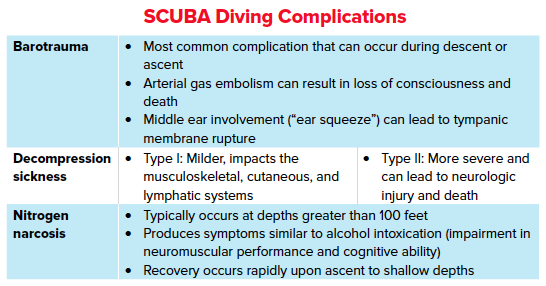
The anatomic location of gas bubbles will reflect symptomology. DCS can be classified based on these clinical manifestations. Type I DCS is the milder of the two, affecting the musculoskeletal, cutaneous, and lymphatic organ systems. The most common manifestation of DCS Type I is localized joint pain ("the bends'').1 The elbow and shoulder are the most often affected joints. Skin manifestations of Type I DCS include pruritus and rash- notably Cutaneous marmorata, a type of skin mottling. Furthermore, lymphatic obstruction can cause lymphadenopathy and diffuse edema.
Type II decompression sickness is the more severe type, affecting the neurologic and cardiopulmonary organ systems. Neurologic symptoms include headache, confusion, numbness, paresthesia, altered mental status, and loss of bladder control. In severe cases it can cause weakness, even to the point of paralysis. When the inner ear is affected, one can experience nausea, vertigo, tinnitus and ataxia. Signs of barotrauma on examination may be evidenced by tympanic membrane rupture. Cardiopulmonary symptoms include chest pain, wheezing, cough and shortness of breath (“the chokes”). Of note, Type II decompression illness is a distinct entity from arterial gas embolism. In arterial gas embolism, rapid ascent without exhalation results in alveolar rupture and subsequent tissue embolization. The classic presentation of arterial gas embolism is a diver who becomes unconscious when resurfacing from the water.
Diagnosis and Management
DCS is a clinical diagnosis, as presentation may be delayed up to 48 hours after the inciting event. No specific investigations will establish its diagnosis. Thus, treatment for patients with DCS should not be delayed for diagnostic workup. Complete blood counts and basic chemistries can be performed to assess fluids status.4 A chest x-ray can be useful as DCS can cause barotrauma resulting in pneumothorax, pneumomediastinum, and pulmonary edema.
The goal in treatment of DCS is nitrogen washout. Initial management should include placing the patient on 100% oxygen via a non-rebreather mask, regardless of their oxygen saturation on pulse oximetry. This will help decrease plasma nitrogen concentration as well as decrease the size of the bubbles.5 Fluid administration at a rate of 1.5 mL/kg/hr will reverse dehydration that is common in divers.6 Definitive treatment of DCS is hyperbaric oxygen therapy. Recompression in a hyperbaric chamber re-shrinks the bubbles, allowing for them to exit the tissue and be filtered out via the pulmonary capillaries. Furthermore, administration of high partial pressure oxygen will increase oxygen delivery to tissues and alleviate ischemic insults that may have been caused by an air embolism.4 Length of treatment in decompression chambers is based on severity of symptoms. Patients who require transfer for hyperbaric therapy should go via ground transport, because air travel can worsen DCS.7 Patients with minimal symptoms who are being discharged should be advised to avoid any air travel for 48 hours.8
Case Conclusion
Because of concern for decompression sickness, we contacted the Divers Alert Network (DAN). Consultation included a description of the presentation as well as a thorough evaluation of the patient's dive profile. It was ultimately determined that the patient be transferred for hyperbaric therapy at the nearest facility.
Take-Home Points
- Careful history-taking in patients with recent SCUBA diving activity can help guide further work-up. Inquire about the depth of descent and timing in which symptoms developed.
- Decompression illness occurs when gas bubbles remain trapped in bodily tissues. Type I is mild while Type II is more severe and can be life-threatening.
- The goal in the management of decompression illness is nitrogen washout. This can be achieved by hydration, supplemental oxygen, and consideration for hyperbaric therapy.
- The Divers Alert Network (DAN) is available for emergent medical assistance when treating patients with suspected diving related diseases.
References
- Cooper, Jeffrey S. Decompression Sickness. 24 June 2020, www.ncbi.nlm.nih.gov/books/NBK537264/.
- Tetzlaff, Kay et al. “Evaluation and management of decompression illness--an intensivist's perspective.” Intensive care medicine 29,12 (2003): 2128-2136. doi:10.1007/s00134-003-1999-1
- Sun, Qing, and Guangkai Gao. “Decompression Sickness.” The New England journal of medicine 377,16 (2017): 1568. doi:10.1056/NEJMicm1615505
- Barratt, Diana Marie et al. “Decompression illness in divers: a review of the literature.” The neurologist 8,3 (2002): 186-202. doi:10.1097/00127893-200205000-00005
- Hardy, K R. “Diving-related emergencies.” Emergency medicine clinics of North America 15,1 (1997): 223-40. doi:10.1016/s0733-8627(05)70292-3
- Muth, C M, and E S Shank. “Gas embolism.” The New England journal of medicine 342,7 (2000): 476-82.
- Cialoni, Danilo et al. “Flying after diving: in-flight echocardiography after a scuba diving week.” Aviation, space, and environmental medicine 85,10 (2014): 993-8.
- Sheffield PJ. Flying after diving guidelines: a review. Aviat Space Environ Med. 1990 Dec;61(12):1130-8.



