A 45-year-old female with a history of hypertension and ulcerative colitis presents to the ED with a headache that started 2 weeks ago and has not gone away. She believes it is because of her high blood pressure (in triage, it is noted to be 200/108). This morning she woke up with numbness on the left side of her face, nausea, vomiting, and difficulty walking. On physical examination, you note a left facial droop, a left pronator drift, and unsteady gait. She is outside your institution’s stroke alert activation window. You obtain a stat head CT, which demonstrates a right thalamic infarction. Given her symptoms, you suspect a possible uncommon cause of her stroke, and perform CT venography, which reveals the presence of cerebral venous sinus thrombosis.
What is cerebral venous sinus thrombosis (CVST)?
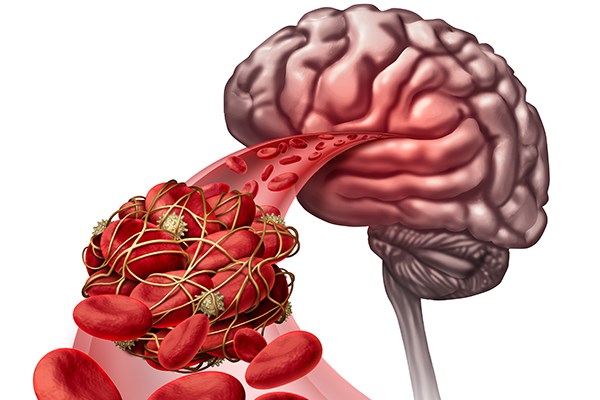
CVST is the complete or partial occlusion of cerebral veins or dural sinuses secondary to an intraluminal thrombus. It is a relatively rare condition, with an annual incidence of 0.2 to 0.5 per 100,0001. It is 3 times more common in women, and is often associated with sinusitis, ear infections, trauma, surgery, hypercoagulable states, medications such as oral contraceptive pills (OCPs), steroids, and hematologic and inflammatory conditions such as ulcerative colitis (UC) and Systemic Lupus Erythematosus (SLE).2
How does cerebral venous sinus thrombosis present?
Headache is the most common symptom associated with CVST. Although the characters of the pain may be variable between individuals, the pain often starts gradually, and progress in severity over a period of days. In some cases, CVST may cause seizures, focal neurological deficits, and may even progress to encephalopathy in severe cases.2-5
How do you work up a patient for suspected CVST?
Patients with suspected cerebral venous thrombosis should undergo venous imaging. The American Heart Association/ American Stroke Association (AHA/ASA) 2011 guidelines indicate that both CT head with venography and MRI head with venography are considered adequate tools for evaluating CVST.6 Although digital subtraction angiography remains the gold standard for the diagnosis of CVST, this is increasingly less utilized given the accuracy of non-invasive imaging.
Several studies have examined the role of d-dimer levels in evaluating patients for CVST.7-9 Although no formal guidelines exist on implementing this into clinical practice, the utility may be strictly limited to low-risk patients,8 as data indicates that d-dimer may inaccurately exclude patients with subacute or chronic disease.9
How do you treat a cerebral venous sinus thrombosis?
Systemic anticoagulation is the mainstay of therapy for CVST. Counterintuitively, this is often the case even in the presence of associated intracranial hemorrhage, although some controversy remains in the literature.
The body of literature is largely limited to 2 RCTS.10 The first one was done in 1991 had to be stopped early due to mortality in the placebo group.11 The second was done in 1999 found no statistically significant difference between anticoagulation and non anticoagulation groups.3 A more recent observational study has shown a lower mortality than has been previously reported, and this is believed to be partly secondary to wider adoption of anticoagulation.2 There is also success reported with thrombectomy or local thrombolytic therapy.12 However, this is generally reserved for severe cases.
Antibiotics should be considered in cases where a concomitant infection is suspected. CSVT patients should be admitted, either to the ICU or step-down unit depending on the severity of their illness.
What is the prognosis of cerebral venous sinus thrombosis?
If left untreated, CVST may progress from headache to seizures, unilateral or bilateral infarction with focal neurologic deficits, to elevated intracranial pressure, herniation and death. In the past, "death or dependency" was reported as high as 39%, however more recently as low as 13%.2 This may be secondary to improved recognition, general improvement of critical care or possibly to wider adoption of systemic anticoagulation in treating CVST.
Summary
CVST is a can’t-miss diagnosis in the ED given its high mortality if untreated. Suspect CVST in patients with gradually worsening headache and focal neurologic deficits, especially if they are high risk (SLE, UC, OCPs, procedures, trauma, or infection). Treatment involves anticoagulation and admission to neurologic care.
References
1. Devasagayam S, Wyatt B, Leyden J, Kleinig T Cerebral Venous Sinus Thrombosis Incidence Is Higher Than Previously Thought: A Retrospective Population-Based Study. Stroke. 2016;47(9):2180-2.
2. Ferro JM. Prognosis of Cerebral Vein and Dural Sinus Thrombosis: Results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004;35(3):664-670.
3. S.F.T.M. de B, Stam J. Randomized, Placebo-Controlled Trial of Anticoagulant Treatment With Low-Molecular-Weight Heparin for Cerebral Sinus Thrombosis. Stroke. 1999;30:484-488.
4. Bousser MG, Russell RR. Cerebral venous thrombosis. In: Major Problems in Neurology, Warlow CP, Van Gijn J (Eds), WB Saunders, London 1997. p.27, 104
5. Agostoni, E. Headache in Cerebral Venous Thrombosis. Neurol Sci. 2004;25 Suppl 3:S206-10.
6. Saposnik G, Barinagarrementeria F, Brown RD Jr, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(4):1158-92.
7. Thammishetti V, Dharanipragada S, Basu D, Ananthakrishnan R, Surendiran D. A Prospective Study of the Clinical Profile, Outcome and Evaluation of D-dimer in Cerebral Venous Thrombosis. J Clin Diagn Res. 2016;10(6):OC07-10.
8. Alons IM, Jellema K, Wermer MJ, Algra A.D-dimer for the exclusion of cerebral venous thrombosis: a meta-analysis of low risk patients with isolated headache. BMC Neurol. 2015;15:118.
9. Hiltunen S1, Putaala J, Haapaniemi E, Salonen O, Tatlisumak T. D-dimer and clinicoradiologic features in cerebral venous thrombosis. J Neurol Sci. 2013;327(1-2):12-4.
10. Stam J, De Bruijn S, De Veber G. Anticoagulation for cerebral sinus thrombosis. Stroke. 2003;34(4):1054-1055.
11. Einhaupl KM, Villringer A, Mehraein S, et al. Heparin treatment in sinus venous thrombosis. Lancet. 1991;338(8767):597-600.
12. Stam J, Majoie CBLM, Van Delden OM, Van Lienden KP, Reekers JA. Endovascular thrombectomy and thrombolysis for severe cerebral sinus thrombosis: A prospective study. Stroke. 2008;39(5):1487-1490.