Identifying ocular infections and potential severity is a critical challenge in the clinical management of patients in the emergency department. Ophthalmology cases are important in the education and management of patient care as randomized, controlled clinical trials in ocular studies are limited and rely on retrospective case studies, case reports, and series.
We present a case in which emergent action was taken with a patient who presented with a significant vision-threatening corneal keratitis (also known as a corneal ulcer) with extended contact lens wear after hot tub use.
Case
A 49-year-old male with a previous medical history of controlled hypertension and tobacco use presented to the emergency department with difficulty seeing from his right eye. The patient reported he had been experiencing pain and difficulty seeing for approximately the past 3 days after using his hot tub. The onset of pain and vision loss was gradual. He stated that he installed a new hot tub; however, he did not chemically treat the water with chlorine or follow through with maintenance of pH balance or alkalinity after filling it with well water.
The patient also reported he was wearing contact lenses while in the hot tub. He stated that his contacts are FDA-approved for extended use and that he had them in for approximately 2 weeks. After using the hot tub, he kept the contact lens in his eyes for approximately 3 days despite increasing discomfort, pain, and difficulty seeing through his right eye.
The patient was discharged from the emergency department with instructions to follow up for specialized outpatient eye care. Following the ED visit where the critical action was made to identify the hypopyon and notify an ophthalmologist for specialized eye care, an ophthalmologist specializing in ocular diseases saw the patient approximately 24 hours later in clinic.
Investigation
Knowledge of potential differential diagnoses of the ocular pathology is essential to start appropriate therapy in order to optimize outcomes.
Investigation of the patient’s head, ears, throat, and left eye was within normal limits and noncontributory. A focused exam of the cheek, nose, and brow was unremarkable. External examination of the right eye and orbit were grossly negative for asymmetry. Visually, the right eye presented with erythema in the conjunctiva and sclera with a remarkable opaque circular disc in the cornea overlying the pupil appearing to be within the mucus, water, and oil layers of the surface, on initial exam.
Focused investigation with a Marco 2b Ultra slit lamp of the right eye was conducted with adjusting the illumination of beam light, on rheostat, to 50% and 10x magnification. Visualization of the eyelid, eyelashes, meibomian glands, palpebral and bulbar conjunctiva, and upper and lower lids was conducted. The conjunctiva and sclera of the anterior globe presented with erythema, positive ciliary flush, which was highly suggestive of anterior uveitis.
The patient reported copious white discharge around his conjunctiva and sclera at night and while he slept. He was advised to not aggravate the infected site and, if in discomfort, he could gently wipe away the access with a clean tissue from the lower eyelid, making sure not to apply pressure to the globe itself for risk of puncture or perforation.
Due to the sensitivity of eye movements, the patient was assessed with gentle and slow movements of the ocular muscles, moving eye medial, lateral, above and below, as well as examination of the upper lid and fornix. The upper eyelids were manually held in place and a cotton-tipped applicator was used to aid movements to minimize discomfort during the exam. No foreign bodies were seen in the eye orbit or within the eye architecture.
Examination of the cornea revealed an extraordinarily significant opaque circular corneal ulcer overlying the pupil, iris, and limbus measuring approximately 3.5mm x 3.5mm in size (seen using a slit lamp in Images 1 and 2). No thinning of the center or borders was appreciated in the dense inflammatory cells forming the hypopyon. The eye was negative for hyphema, or other hematologic pathology. The illumination was shifted to an oblique angle, using a narrow beam to produce the recommended optical cross section of the cornea. This technique, as outlined by Allen and Parker, allows for partial reflection as the light passes through the tear film, epithelium, stroma, descemet’s membrane, and endothelium.1
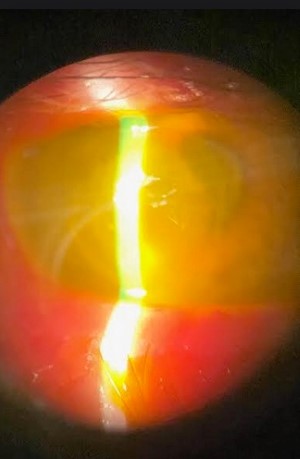
Image 1: First presentation of corneal ulcer, right eye

Image 2: Approximately day 4 corneal ulcer, right eye
Using this method, the presence of keratic precipitates were appreciated on the internal endothelium of the inner surface of the cornea toward the anterior chamber and were evident on the farthest layer from illumination. Careful slow sweep of illumination was conducted from temporal to medial nasal sites, using vertical slit beam and then with cobalt blue filtered light using a fluorescein stain without other irregularities except as otherwise discussed above. Fluorescein staining showed significant keratitis of the right eye (Image 3).
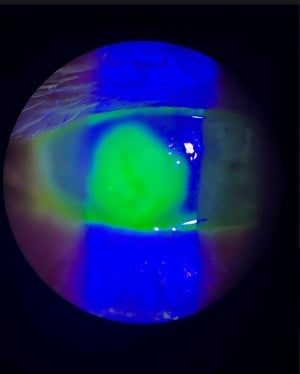
Image 3: Day 14 of right-eye corneal ulcer
The patient was instructed to not wear contact lenses until the infection of his eye had improved. The patient was advised to wear his regular glasses as needed. Instructions for the management of the excessive discharge included to refrain from rubbing the eye or from putting liquids or materials other than the prescribed medications into the right eye. It was also recommended that the patient not use his hot tub without the recommended water treatment due to the potential for the water source to contain infectious organisms and contaminants.
Due to the vision-threatening status of the patient’s eye and severity of case presentation, the patient was aggressively medically managed with ciprofloxacin 0.3% ointment before bedtime and oral ciprofloxacin 500 mg twice a day. In addition, for the first 2 weeks, the patient alternated between gentamicin 0.3% and moxifloxacin 0.5% topical eye drops every hour around the clock. On day 3, prednisone acetate 1% twice a day was started. After approximately 3 weeks, the regimen was decreased to alternating the gentamicin and moxifloxacin drops to every 2 hours. At that time, the steroid was increased to 3 times a day. Approximately 6 weeks after initial presentation to the clinic, the patient was started on moxifloxacin and tobramycin 4 times a day, and erythromycin ointment 0.5% for management of corneal toxicity, discussed further below.
The patient followed up daily in the clinic for the first 2 weeks, then biweekly and weekly thereafter. On day 2 of presentation to the clinic, the patient reported he had drained and emptied the hot tub and it was no longer in use. Over the course of 2 weeks, the patient’s corneal ulcer remained stable without worsening symptoms or growth of ulcer. There was minimal change in size to the ulcer over the first week. Potential differential diagnoses were discussed and investigated. They included, but were not limited to, Acanthamoeba keratitis, petrifying pseudomonas secondary to Pseudomonas aeruginosa infection, herpetic keratitis, and mycotic keratitis.
With the patient’s improvement with aggressive treatment and close monitoring, case assessment, and case history, the working diagnosis of corneal ulcer secondary to pseudomonas aeruginosa was made. Continued care and management of the patient’s eye was discussed, with emphasis on the critical importance of continued adherence to the therapy regime. Further, future considerations for corneal transplant with an amniotic graft using stem cells was discussed with the patient, as well as the possibility of complete loss of vision in the eye. Discussions such as these can be emotionally upsetting. However, all potential outcomes need to be discussed with patients, as was done in this case.
Discussion
The slit lamp is formally known as a stereoscopic biomicroscope that emits a focused beam of light with variable height, width, and angle that allows for 3D visualization and measurement of the anterior segment and adnexa of the eye.2 When used with handheld lenses, the poster segment of the eye can also be visualized. The use of slit lamps for ophthalmology cases in the ED is the mainstay of eye examinations.3 It is critical for EM residents and emergency physicians to understand the function and operation of a slit lamp in order to allow for a complete and accurate examination in the ED (Image 1). Although literature investigating the classification of different corneal ulcer types has been pursued previously,4 disseminating research to physicians and into clinical practice among the non-ophthalmological specialties may still be lacking.
The World Health Organization previously reported that about 6 million people around the world are affected by cornea-related blindness or moderate/severe visual impairment.5
Hot tubs and jacuzzis are popular forms of recreation and relaxation in the United States and provide health care benefits such as stress and muscular tension release, lower blood pressure, and improved sleep. The more commonly known pseudomonas infections associated with hot tubs and water sources include hot tub folliculitis, otitis externa, and varicose ulcers; these infections are mostly superficial and not life- or organ-threatening. Humidifiers6 and whirlpools7 are also sources of contamination and disease risk.8 There are only a few published reports of severe P. aeruginosa infections occurring in previously healthy persons without underlying diseases.12 Other disease processes, such as acute prostatitis and urosepsis after sexual relations in a hot tub, have previously been reported.9
Ocular infections, including keratitis, pose a high risk for permanent vision loss and scarring. Therefore, management is time-sensitive, emergent medical care is critical, and identification of disease is imperative in the ED. Ocular infections are often difficult to pinpoint due to the availability of specialized resources, training level of care-givers, and lengthy time requirements to culture ocular strains. Cases such as this one are time-sensitive, and immediate aggressive management will assist in preserving some, if not all, eye function.
Usually, corneal infections are assumed to be bacterial until proven otherwise by laboratory studies or until a therapeutic trial is unsuccessful.10 Major common organisms that emergency physicians and medical students need to be aware of are Staphylococcus, Streptomonas, Moraxella, and Serratia. In addition, in similar case presentations,consider Acanthomoeba, a common parasitic organism in the environment, and Pseudomonas Aeruginosa, a bacteria that adheres to and infiltrates the cornea. Both Acanthomoeba and Pseudomonas are found in soil, swimming pools, hot tubs, and freshwater bodies (ponds, lakes, creeks). Warm water in hot tubs, particularly untreated water, is naturally conducive to the growth of thermophilic organisms. Prompt action in initial treatment with broad spectrum therapy is critical, as was displayed in this case.10
This patient presented to the clinic with a classic presentation of pseudomonas keratitis with a rapidly progressive, suppurative infiltrate with a hypopyon and mucopurulent discharge after extended contact lens and hot tub use as well as ocular pain, photophobia, decreased vision, discharge, and inability to wear contact lenses. In comparison to common presentation of Acanthamoeba infections, the infiltrate in this case was a focal white opacity in the corneal stroma with stromal loss and overlying epithelial defect which stained with fluorescein, indicating an ulcer. In addition, the infiltrate was densely opaque without the ability to visualize beyond the ulcer to the iris.
Although the patient did not present with the signs of an acanthamoeba infection, it was a consideration as a differential diagnosis, which requires time to deduce. This is among the challenges in diagnosing patients in the ED,where length of time to monitor over extensive periods while aggressively treating organisms is crucial to patient care.Patients with Acanthamoeba keratitis are often highly compromised due to extremely severe and persistent ocular pain as well as vision loss. Often, the protozoa will infiltrate the keratin and stromal layers and create a ring-shaped infiltrate in weeks 3 to 8. On slit lamp, the appearance of the corneal protozoan is more HSV in character rather than a bacterial ulcer.10 Patients will require extensive time for treatment and healing as well as meticulous monitoring and frequent follow-up visits, as seen with this patient. Patients may require other invasive surgeries, including corneal grafts, which may interfere with the quality of a meaningful personal and professional life.11 Although rare, fatalities due to hot-tub-associated Pseudomonas aeruginosa infections are possible, as previously reported in literature in a case involving a healthy woman with a contaminated hot tub.12
The patient had reported he drained the hot tub of water and that it was no longer in use. Although this knee-jerk proactive measure ensured he and no one else would be in contact with the infectious contaminants in the water, this also hindered the case by making it difficult to investigate organisms in the water source. The ability of culturing and isolating water samples for screen and subtyping isolates as recommended by many states13 was not possible in this case.
The EMRA Antibiotic Guide outlines basic treatment and dosing requirements for corneal abrasions for contact lens and non content lens wearers before progression to ulcers.14 Physicians should be made aware of safely preserving water samples for containment testing, as well as encouraging the exercising of caution in homes with hot tubs and children.In this case, extra care was taken to minimize aggravation or provocation of the eye with invasive instrumentation in order to offset any potential of puncturing or perforating the fragile cornea. Daily monitoring by an ophthalmologist was critical in attempting to preserve this patient’s eyesight. Furthermore, some patients may delay seeking care as they are unaware of the risk of permanent vision loss or potentially life-threatening nature of these ocular infections. Often, this delay in care increases the severity of the disease process.
Take-Home Points
- Corneal ulcers from infectious agents, such as Pseudomonas aeruginosa and Acanthomoeba from water sources such as hot tubs and pools, can be vision-threatening — especially in cases involving extended-use contact lenses. Knowledge of presentation and signs is important when differentiating between these two organisms.
- Daily evaluations for vision-threatening ulcers are critical, as is measurement of the size and shape of infiltrated space.
- Patient education about hot tub ownership, maintenance, and safe operation is an important preventative health care measure. Patients with hot tubs should be advised regarding weekly maintenance with water-treatment formulas (at minimum), chemical treatments, and the cost, time, and effort necessary for safe hot tub use. The risks of not maintaining hot tubs and pools, koi ponds, and other man-made water bodies involve infections with organisms such as pseudomonas.
- The general public may be unaware of public health concerns with water treatment and possible infectious organisms in their geographic areas.
- Despite FDA-approved contact lenses for extended wear, patients may be unaware of the individual personalized care necessary for their own extended use, including in activities such as hot tub use.
- EM residents and health care providers should be aware of long-term use of steroids and antibiotics in patients treated for corneal ulcers. Potential risks include corneal toxicity. Awareness of this side effect is crucial in order to alternate with other necessary antibiotic and medical therapy for ongoing care. Pain management is also recommended in patients with a corneal ulcer.
- Health care providers should be aware of the emotional and psychological strain that long-term management of a corneal ulcer may have on the patient and family. Waking up to administer eye drops will affect sleep patterns. Patients may have anxiety for the long-term effects if there is a complete loss of vision in one eye. Quality of life may decrease with inability to enjoy normal activities. This can be difficult to process and may require gentle reassurance and compassionate care.
References
- Allen, R. C. & Parker, R. A. Basic Ophthalmology: Essentials for Medical Students. 10th Ed, (American Academy of Ophthalmology, 2016).
- American Academy of Ophthalmology: https://www.aao.org/ [accessed on 8/2/2023]
- American Academy of Ophthalmology: https://www.aao.org/ [accessed on 8/2/2023]
- Alquran H, Al-Issa Y, Alsalatie M, Mustafa WA, Qasmieh IA, Zyout A. Intelligent Diagnosis and Classification of Keratitis. Diagnostics (Basel). 2022 May 28;12(6):1344. doi: 10.3390/diagnostics12061344. PMID: 35741153; PMCID: PMC9222010.
- World Health Organization: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment. [accessed on 9/12/2023].
- Huhulescu, S., Simon, M., Lubnow, M. et al. Fatal Pseudomonas aeruginosa pneumonia in a previously healthy woman was most likely associated with a contaminated hot tub. Infection 39, 265–269 (2011). https://doi.org/10.1007/s15010-011-0096-6.
- Rose HD, Franson TR, Sheth NK, Chusid MJ, Macher AM, Zeirdt CH. Pseudomonas pneumonia associated with use of a home whirlpool spa. JAMA. 1983;250:2027–9.
- Pier GB, Ramphal R. Pseudomonas aeruginosa. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases, 7th edn. Philadelphia: Churchill Livingstone Elsevier; 2010. p. 2835–60.
- Dulabon LM, LaSpina M, Riddell SW, Kiska DL, Cynamon M. Pseudomonas aeruginosa acute prostatitis and urosepsis after sexual relations in a hot tub. J Clin Microbiol. 2009 May;47(5):1607-8. doi: 10.1128/JCM.02376-08. Epub 2009 Mar 18. PMID: 19297589; PMCID: PMC2681869.
- Bagheri, Nika, et al., editors. The Wills Eye Manual. 5th ed., Lippincott Williams and Wilkins, 2008., Page 63.
- Varacalli G, Di Zazzo A, Mori T, Dohlman TH, Spelta S, Coassin M, Bonini S. Challenges in Acanthamoeba Keratitis: A Review. J Clin Med. 2021 Mar 1;10(5):942. doi: 10.3390/jcm10050942. PMID: 33804353; PMCID: PMC7957573.
- Huhulescu, S., Simon, M., Lubnow, M. et al. Fatal Pseudomonas aeruginosa pneumonia in a previously healthy woman was most likely associated with a contaminated hot tub. Infection 39, 265–269 (2011). https://doi.org/10.1007/s15010-011-0096-6.
- Dulabon LM, LaSpina M, Riddell SW, Kiska DL, Cynamon M. Pseudomonas aeruginosa acute prostatitis and urosepsis after sexual relations in a hot tub. J Clin Microbiol. 2009;47:1607–8.
- Levine, EMRA Antibiotic Guide, 20th ed., EMRA, 2022., Page 32.



