The Patient
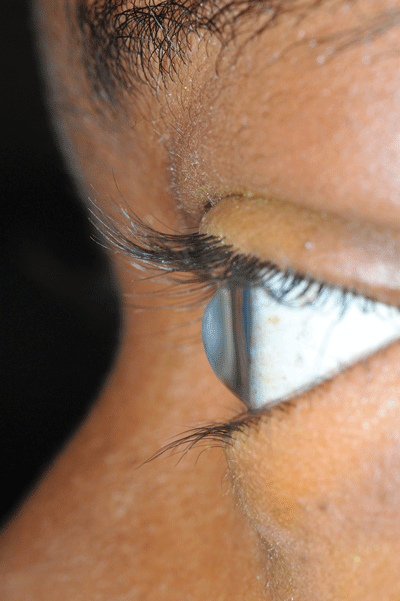
A 36-year-old female presents to the emergency department with 1 week of decreased vision, pain, and photophobia of her left eye. She denies any precipitating factor. She has known bilateral keratoconus with corneal transplant of the right eye. Visual acuity is hand motion only in the left eye, and 20/25 in the right eye. Examination is notable for central corneal opacity of the left eye (Image 1). There is no uptake with fluorescein stain.
What is the diagnosis?
Corneal opacity without fluorescein uptake in a patient with keratoconus is most consistent with corneal edema (called corneal hydrops), a consequence of keratoconus. Keratoconus is a non-inflammatory eye disorder characterized by progressive thinning of the cornea leading to a cone shaped deformity (Image 2). This condition typically presents at puberty or early adulthood with blurry vision or a sudden decrease in visual acuity. Munson's sign, a V-shaped indentation of the lower eyelid on downward gaze caused by a protruding cone (Image 3), is seen in advanced disease. Risk factors include systemic disorders such as Down syndrome, Ehlers-Danlos syndrome, and osteogenesis imperfecta. Eye rubbing, contact lens use, and family history also may put patients at risk. Initial treatment of keratoconus is with standard corrective lenses. As symptoms progress, patients will typically require specialized contact lenses for refractive correction, and may ultimately require a corneal transplant.
Corneal hydrops is a complication of advanced keratoconus and is characterized by sudden onset of severe corneal opacification because of edema. The edema occurs from a spontaneous break in Descemet's membrane because of the weakened cornea, leading to a sudden and painful decrease in visual acuity. There is no specific treatment for corneal hydrops, and the symptoms generally resolve over several months. Our patient was treated with prednisolone acetate ophthalmic suspension to reduce inflammation and provided cornea specialist follow-up.
All photos courtesy of Lawrence B. Stack, MD