As new interns embark on the path towards becoming EM physicians, many may be surprised (and sometimes frustrated) to realize the sheer volume of patients who may not meet any criteria for urgency in their visits. Now, in my third year of residency, I think I've heard it all when it comes to making sense of this national dilemma. And much of it comes down to access: Non-emergent patients turn to the ED when they don't have any other access to a doctor at the time, place, and cost that suits their socio-economic status.
Besides access, education and emotion both play a role in a patient's decision to visit the ED. Often intertwined, both speak to a particular culture that is reinforced in the dramatization of health. An example might be the person who comes because their friend or relative has a serious condition and it began in very much the same way as they are now perceiving their own symptoms. Probably the most frustrating for residents is the otherwise asymptomatic, first-trimester vaginal spotters. With the rate of ectopic pregnancies being so low and the rate of this particular symptom being so high, the extent to which we work up these patients can become an acute point of frustration.
Finally, we have what I like to think of as our public service patients: those who show up for a warm or cool place to stay for a few hours, perhaps a meal, and even perhaps a fix. These patients have found a second home in our always-open department. Eventually, one may come to appreciate them perhaps for the mere fact that they're the only population of patients in the ED more than you. In this group, I may also count the patients who are ushered to the ED for an inpatient admission without any need for ED stabilization. The downstream systemic effects of what appear on the surface to be benign practices can be crippling.
Interestingly, rationales may be perceived differently by providers on this issue. On the provider side, we have recognized that the patient who doesn't necessarily need to be in the emergency department receives sub-optimal care (e.g. a battery of tests for the most dangerous things without ever resolving the actual thing) and yet we never turn away a patient. Even the semblance of turning away a patient by doing something simple like adding an expected wait time is sometimes frowned upon. The reason often cited by providers and ED administrators is EMTALA and medical malpractice liability. There are a number of ways to dissect this issue further, and many smarter people have. Especially as a trainee, the fact of the matter is that any judgment on our part on the validity of the emergent nature of a visit may bias our medical decision-making and lead to misses. When patients step into the ED, for better or for worse, we are there for all of them.
Patients continue to turn to the ED even when they recognize their symptoms do not constitute a medical emergency. Though we know it's a problem, we, as a community, lack data that can help clarify this issue. We know the ED is a safety net for all people and outpatient health care is a complex beast that stumps even the educated. In this day and age, we should have better data on the exact percentage of visits that are deemed to be appropriate for an ED visit versus those that would be more appropriate in an outpatient setting. In addition, we should be able to identify and quantify why this misstep happened.
The Emergency Severity Index (ESI) is a tool that is currently used to classify patient visits by disease and resource intensity in almost all EDs in the country. It resembles a medical evaluation, which is characteristically apart from the actual distinguishing factors that separate emergent from non-emergent visits. We know all these patients need a doctor, and sometimes they may need a lot of resources, but in my experience, the young “chest pain for many months” patient can get classified to be more appropriate of an ED visit than a suspected broken bone.
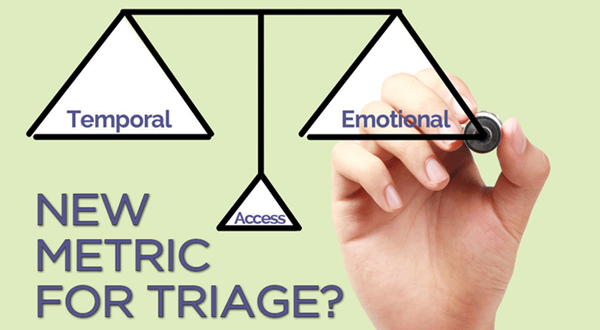
A new classification system or metric is in order that can help further our knowledge in this area and advocate for our patients more effectively. Realizing that reasons why patients with non-emergent symptoms come to the ED are actually secondary to socio-economic, educational, or emotional reasons, I propose the new new metric displayed below.
Temporal Questions
3 points related to the temporal nature of the issue:
0 I've had this problem for a few months and/or there is no change or anticipated change in my symptoms.
1 I've had this problem for a few weeks and/or it just began to change slightly.
2 I started having this problem in the last few days and/or it has begun to evolve.
3 I just began having this problem and/or I believe this problem is evolving rapidly.
Emotional Questions
3 points related to the emotional component of the patient's symptoms:
0 I have no fear that this issue will cause any immediate threat to my health, and I might have waited a week to be seen if I could get an appointment.
1 I fear that this issue will lead to a bigger issue if I don't get treatment in the next few days.
2 I fear for a lengthy illness if I don't get treatment in the next few hours.
3 I fear for my (or my dependent's) life if I don't get treatment within the next few hours.
Access Questions
3 points related to the economic component of the patient's symptoms:
0 I do not have a doctor or cannot go to a doctor because I have no mode of transportation, or no time to get there, or I don't have money to go to an office doctor.
1 I have a doctor but I cannot get an appointment when needed (including after business hours) or I cannot get transportation when needed.
2 I have a doctor but he or she is on vacation or otherwise temporarily unavailable.
3 I have a full set of doctors whom I can see as needed.
Min score: 0, Max score: 9
To protect from the unintentional consequences, it could be immediately anonymized and remain hidden from the patient's chart.
How would this help?
Ideally, we would have a more quantitative and specific way to detail the degree to which we serve as a safety net for America. Sometimes, I find myself wondering what our departments would be like if we only saw the true emergency cases. Would our patients get better, less rushed care? Would our decision making criterion become more sensitive and specific? Would our patient satisfaction improve? Would our number of misses and near misses decrease? If we get any closer to any of these goals, then I believe it will be worthwhile.