The bag-valve-mask (BVM) is ubiquitous and highly utilized in all fields of emergency care.
Yet despite its seemingly intuitive operation and perceived simplicity, the BVM is an overlooked and misunderstood component of high-quality critical care and resuscitation.
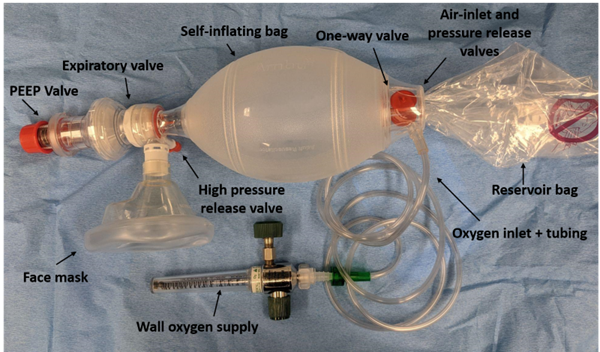
Components of a BVM
First, let's start by understanding the components of the BVM.
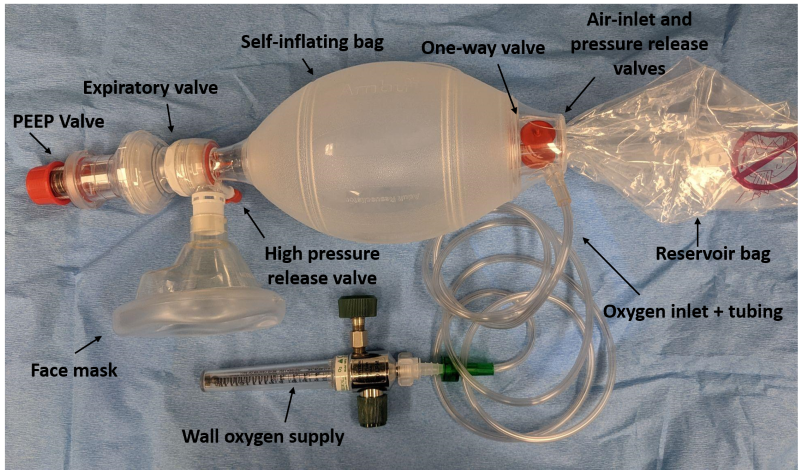
Figure 1. Anatomy of the BVM, with each component labeled
What Does It Do?
- Provide PEEP and high FiO2
- Augment a patient's spontaneous ventilation
- Manual ventilation of an apneic patient
How Does It Work?
The BVM only functions as intended with high rates of oxygen flow, a patent airway, and a good mask seal. To get true continuous positive airway pressure (CPAP), it must also be combined with a peep valve and a nasal cannula (see "PEEP/CPAP" below).1 When those conditions are met, it can deliver true 100% FiO2 with continuous positive end-expiratory pressure (PEEP). Connect the BVM to wall oxygen and turn the oxygen knob fully counter clockwise (see "flush rate" below). Maintain a patent airway through patient positioning and airway adjuncts. Common patient positioning involves the sniffing position, head-tilt-chin-lift, or jaw thrust. Regardless the emphasis should be on raising the jaw to the mask rather than pushing the mask posteriorly into the face. Adjuncts to maintain airway patency include the oropharyngeal airway (OPA) or a nasopharyngeal airway (NPA). Edentulous patients should have their dentures left in, or otherwise have their buccal mucosa supported (one study found gauze and an OPA adjunct was most effective).2 Anticipate difficulty obtaining a good mask seal in patients who are obese, older, retrognathic, and with facial hair.
The mask on a standard BVM does not seal itself to the face. It is possible to utilize a mask with straps (eg, a BiPAP mask), but this is not standard practice. As more ventilators are manufactured with the ability to perform both BiPAP and invasive ventilation, it may become more common in the future to use this type of mask for preoxygenation with BiPAP, and then transition to BVM as needed to assist ventilation in preparation for intubation. When using a strapless mask, the airway clinician should ideally hold the mask seal with both hands (figure 2A, 2B) as another rescuer depresses the bag.2 All clinicians perform dramatically better with a two-handed seal, but in one lab experiment, female clinicians were 8 times more effective with a two-handed seal, in contrast to men, who were less than twice as effective with two hands.3 They noted females had shorter, narrower, and weaker hands, but did not perform a multivariate analysis to see if these factors accounted for this difference. A poor mask seal leads to a loss of tidal volume, FiO2, and PEEP resulting in worsening ventilation and oxygenation. A loss of airway patency during ventilation results in stomach insufflation and increased aspiration. Understanding these concepts should reinforce the importance of the two-handed seal and maintenance of airway patency as a component of oxygenation and not just ventilation.
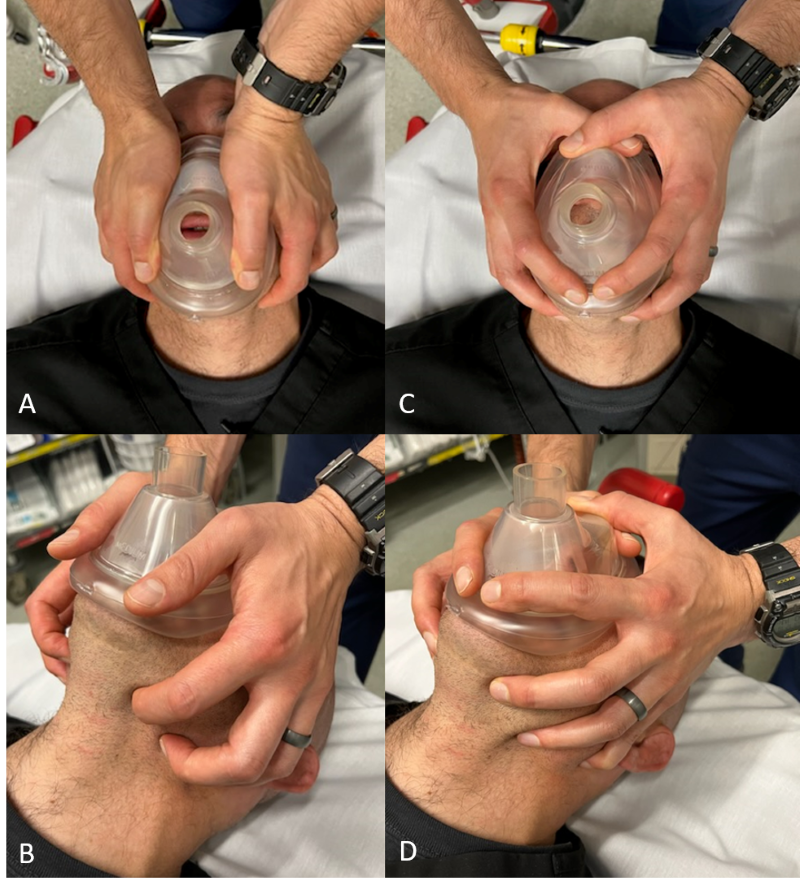 Figure 2. Two-handed grip positions: Figure 2A and 2B is the “two thumbs down” technique. Figure 2C and 2D is the “two-handed C-E” technique. For a BVM to function well, you must 1) maintain airway patency 2) ensure a tight seal
Figure 2. Two-handed grip positions: Figure 2A and 2B is the “two thumbs down” technique. Figure 2C and 2D is the “two-handed C-E” technique. For a BVM to function well, you must 1) maintain airway patency 2) ensure a tight seal
The ability for BVM to apply PEEP or function for CPAP is contingent on the PEEP valve, which is not pre-attached to most BVMs. Learn where they are at your institution before you need one. When attached, this adjustable spring-loaded exhalation valve provides variable resistance that must be overcome to release gas from the lung. It functions similarly to other applications of PEEP apart from one major caveat outlined in the next paragraph. Using a BVM for CPAP decreases alveolar collapse at the end of expiration and improves shunt. This has multiple benefits including improved oxygenation while reducing driving pressure and atelectrauma. Bear in mind the effects of PEEP you have learned about in vented patients. It has hemodynamic effects, particularly at high levels (>15 cm H20), which can be helpful (decreased left ventricular afterload is lifesaving in sympathetic crashing pulmonary edema), or harmful (increased right ventricular afterload and decreased preload can jeopardize a struggling right ventricle). PEEP is generally protective against iatrogenic lung injury, especially among patients with consolidation or infiltration, however, in patients with very poor lung compliance (pulmonary fibrosis, fibroproliferative phase of ARDS), high levels of applied PEEP could lead to barotrauma. In the words of William Owens, if the chest X-ray has white stuff where it should be black, it's generally a good idea to use at least some PEEP.4
In order for BVM PEEP to function as desired (continuous consistent PEEP throughout the respiratory phase) it must be combined with an underlying nasal cannula. Otherwise, there is inadequate pressure in the airways and the PEEP falls towards zero very quickly after the initial phase of expiration. The nasal cannula tubing running underneath the mask is generally not an issue for mask-seal, especially with a two-handed seal.
Indications:
- Provide or assist ventilation
- Provide CPAP
- Provide 100% FiO2
What Can Go Wrong?
Suffocation: Non-self-inflating bags like the Mapleson can effectively deliver "blow-by" oxygen, but the self-inflating BVMs of the emergency department do not. Usually, clinicians will squeeze the self-inflating bag when using a BVM. However, even without depressing the bag, the BVM can be a great way to administer nearly 100% FiO2 with CPAP within seconds of identifying a clinical need and without additional staff (respiratory therapist) or equipment (portable ventilator). This is possible with one crucial caveat: patients may not be able to breathe spontaneously with a BVM on their face if they are very weak or tired. The "exhalation" valve (duckbill valve on the patient end of the bag) may have greater resistance than a patient can overcome with their own inspiratory force. If you see that duckbill valve opening, the reservoir bag deflating slightly with inspiration, and their vitals and appearance are consistent with ventilation, then they are probably overcoming that small resistance on their own. If this is not the case, unless the clinician depresses the bag, they are effectively holding a pillow over the patient's face. This is especially important if using a mask with straps. Therefore, the clinician should always be ready to "assist" the spontaneously breathing patient (by squeezing the bag).
Failure to recognize a non-patent airway: It can be difficult to assess airway patency and mask seal in a loud and hasty resuscitation. Just as we err on the side of consistent first-attempt effectiveness with mask seal by using a two-handed grip, we suggest a similar approach to airway patency. If you anticipate or encounter issues with airway patency, apply an airway adjunct (NPA, OPA). Maximal adjunct usage is one NPA in each nostril and an OPA in the mouth. Successful ventilation and oxygenation are only possible in a fully patent airway. A helpful adjunct worth considering for monitoring the effectiveness of your ventilation is end tidal CO2 waveform capnography (ETCO2). The ETCO2 value may not be accurate, especially when using flush rate oxygen or with an imperfect seal, but trends and waveform morphology can help confirm adequate ventilation and an adequate seal.
Accidental delivery of atmospheric air: Generally, the BVM is hooked up to 100% FiO2; however, lesser concentrations can be inadvertently delivered in the following scenarios:
- Mask leak entrains ambient air: Use both hands to hold a mask seal.
- Ventilation exceeds flow of oxygen delivery: Use high flow rates, generally greater than 15L/min. Wall oxygen is capable of 30 to 60 L/min when the knob is turned fully counterclockwise, despite the gauge capping out at 15L/min. This fully open position is called "flush rate oxygen." Spontaneous ventilation in a sick patient with a high minute ventilation at too low of a flow will result in atmospheric air delivery and lower than intended FiO2. Assisting ventilations decreases this effect. Certain designs of BVM are particularly susceptible to entrainment of atmospheric air.
- Collapsed reservoir bag: This often happens at the start of ventilation or with inappropriately low flow. The self-inflating bag always re-expands after every time its squeezed, either from the reservoir or from the atmosphere. The reservoir bag should be plump, so the gas you give your patient is coming from there and not the atmosphere.
Delivery of excessive volume: The adult BVM delivers >1.5L of gas when fully depressed, which at 8 ml/kg predicted body weight is appropriate for a >10-foot-tall male. One study using a test lung actually demonstrated superior ventilation with a pediatric BVM.5 Adults will generally require 1/3 or less of the adult BVM's volume (less still in most cardiac arrest or ARDS patients).
Delivery of excessive pressure: Excessive inspiratory or expiratory pressure can be harmful. The lower esophageal sphincter opens at about 20 cm H20 in most living patients and around 5 in patients in cardiac arrest. Therefore, using a BVM with excessive PEEP or inspiratory pressure in a living patient can cause stomach insufflation, as can almost any ventilation in an arresting patient, which is partly why supraglottic airway or advanced airways are beneficial in cardiopulmonary resuscitation (CPR).6 At pressures much greater than that, usually around 40 cm H20, a pop-off valve will open on most BVMs. It can be disabled, but this is like silencing a high-pressure alarm on the vent; only do it if it is clinically reasonable.
Design equity: The BVM is sized most appropriately for an adult male patient and rescuer, most training takes place on adult male mannequins, and the test lungs utilized in pulmonary and airway research are patterned on a prototypical adult male. These sex differences set all clinicians and patients up for worse outcomes when these tools are applied to the entire patient population. To combat this, you should use a two-handed grip, minimize excessive volume and pressure, learn sex differences in respiratory anatomy and physiology, and encourage equity in research and design.
Use as a ventilator: The BVM can be used as the foundation for a primitive ventilator. There was a surge of interest in engineering a low-cost and widely accessible ventilator to meet an anticipated need throughout the COVID-19 pandemic. Many of these designs are open-source and result in do-it-yourself ventilators costing only several hundred U.S. dollars.
Take-Home Points
- Use a two-handed seal for effective ventilation and oxygenation.
- Use "flush-rate" oxygen to deliver high FiO2 and flow during inspiration.
- Use a PEEP valve and underlying nasal cannula for effective CPAP.
- Do not use excessive volume or pressure, as these can cause barotrauma and unnecessary stomach insufflation.
References
- Weingart S. Preoxygenation, Reoxygenation and Deoxygenation. EMCrit.
- Golzari SEJ, Soleimanpour H, Mehryar H, et al. Comparison of Three Methods in Improving Bag Mask Ventilation. Int J Prev Med. 2014;5(4):489.
- Otten D, Liao MM, Wolken R, et al. Comparison of Bag-Valve-Mask Hand-Sealing Techniques in a Simulated Model. Ann Emerg Med. 2014;63(1):6-12.
- Owens W. The Ventilator Book. 3rd ed. First Draught Press: Middletown, Delaware; 2021.
- Kroll M, Das J, Siegler J. Can Altering Grip Technique and Bag Size Optimize Volume Delivered with Bag-Valve-Mask by Emergency Medical Service Providers? Prehospital Emerg care. 2019;23(2):210-214.
- Gabrielli A, Wenzel V, Layon AJ, Von Goedecke A, Verne NG, Idris AH. Lower Esophageal Sphincter Pressure Measurement during Cardiac Arrest in Humans: Potential Implications for Ventilation of the Unprotected Airway. Anesthesiology. 2005;103(4):897-899.