BCVI is a relatively rare diagnosis, but this does not take away from the importance of considering it during the initial evaluation of all trauma patients.
Blunt injuries to the carotid or vertebral arteries, collectively referred to as blunt cerebrovascular injuries (BCVI), may be clinically silent at first, but the implications can have devastating effects for patients. BCVI is associated with increased incidence of stroke if not identified in a timely manner and treated appropriately. Mortality may even reach as high as 43%.1 The purpose of this review will be to discuss the relevant anatomy, imaging modalities, grading of injuries and subsequent treatment.
Anatomy
The cerebrovascular system can be divided into the anterior and posterior circulation, supplied by the carotid and vertebral arteries respectively. The common carotid arteries (CA) bifurcate into the internal carotid artery (ICA) and external carotid artery (ECA) at approximately the level of the third and fourth vertebral bodies. The ICAs are then further divided into four segments based upon their anatomic location: cervical, petrous, cavernous, and cerebral. The significance of these segments relates to the potential for injury with certain skull fracture patterns due to the anatomical constraints of the ICA. The vertebral arteries (VA) travel in the vertebral foramina of the sixth through second cervical vertebrae, and are also divided into four segments based on their anatomic location in relation to the cervical spine and skull base.2
Incidence, Injury Pattern, and Screening
BCVI is a relatively rare diagnosis, but this does not take away from the importance of considering it during the initial evaluation of all trauma patients. One study has found the incidence of BCVI to be only 0.64% of admitted blunt trauma patients, but other studies have reported an incidence as high as 2.5%. The CAs or VAs were equally likely to be involved, with mortality being higher when the CAs were involved.1
Injuries are felt to be caused by cervical hyperflexion/extension causing a stretching of the vessels, but injuries may also occur with fractures/ dislocations of the cervical vertebrae lacerating the vessels or direct cervical blows.3
Because of the low incidence of BCVI, emergency physicians must have a high suspicion in order to recognize this dangerous diagnosis with these injury patterns. Patients may present to the ED initially with symptoms of stroke due to BCVI; however, more commonly there is a latent period with symptoms developing 10-72 hours after injury.4
Various trauma institutions have attempted to develop screening guidelines, with one of the most highly utilized being the Denver Grading Scale for BCVIs.5 The Denver group has developed recommendations to screen for BCVI in high-risk patient populations, identified in Table 1.
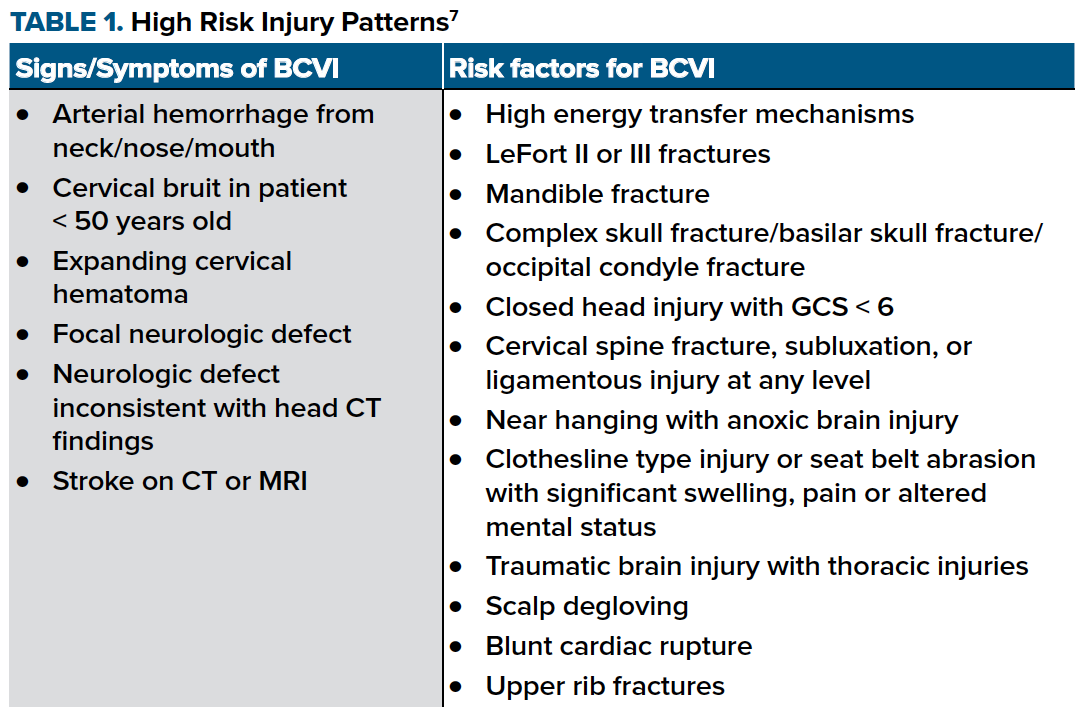
Of these risk factors, skull base fractures have been identified as the highest risk traumatic injury associated with BCVI.6
Imaging
Many imaging modalities exist to help evaluate BCVI including CT-angiography (CT-A), arteriography, magnetic resonance angiography (MR-A), and duplex ultrasonography. CT-A has been recommended as the best screening modality for BCVI in trauma patients. Arteriography can provide a definitive diagnosis; however, it is invasive, has limited availability, and is not ideal to obtain from the ED. CT-A is not perfect, with a sensitivity of approximately 80% and specificity of 97%, but it has been deemed the most cost-effective screening strategy to prevent strokes. MR-A and duplex have no data to support their use as screening modalities for BCVI.2
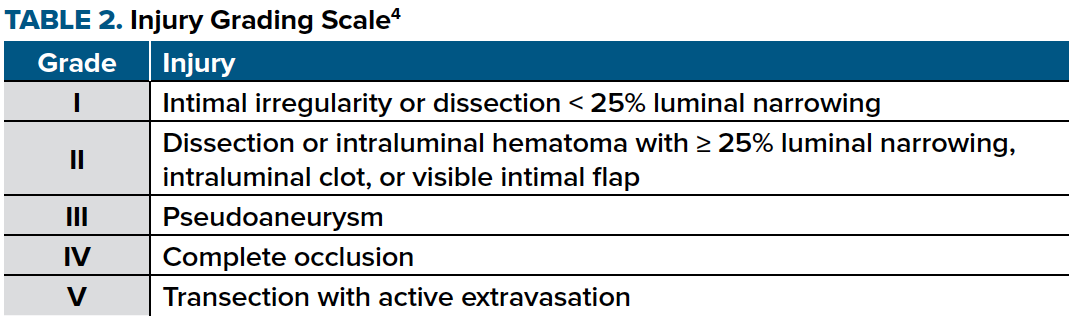
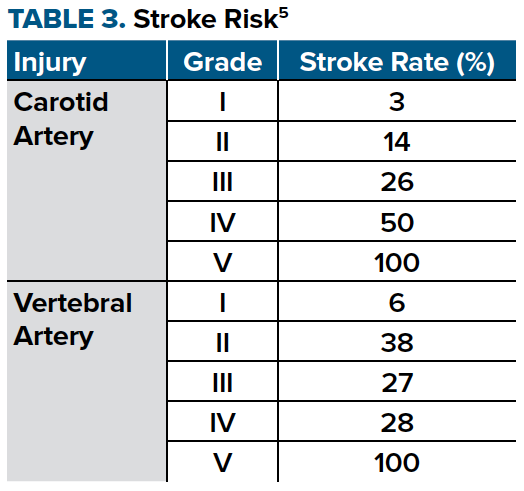
Pathophysiology and Stroke
Injuries to the cerebrovascular system typically cause intimal disruption regardless of the mechanism. This intimal tear then becomes a source for platelet aggregation that has the potential to cause downstream effects such as embolic stroke or vessel occlusion.4 A grading scale has been developed to provide a description of injury as well as categorize the associated stroke risk, seen in Tables 2 and 3.
Treatment Options
Because of the risk of stroke in these patients, treatment with antithrombotics, operative repair, or endovascular stenting is important and may decrease the stroke rate considerably. Antithrombotic agents, primarily heparin, are utilized to promote clot stabilization with prevention of further vessel thrombosis and promotion of resolution via intrinsic fibrinolysis and are extremely effective at preventing stroke.5 Difficulty arises, however, when many of these patients have multisystem trauma and are not amenable to systemic anticoagulation therapy due to bleeding risks.
Operative therapy may not be an option in patients who have vascular injuries in inaccessible areas such as the carotid canals or vertebral foramen; therefore, endovascular stenting may also be considered.
Grade I injuries only require antithrombotic treatment while Grade V injuries require operative repair, via open or endovascular techniques. Grade II-IV injuries may be considered for operative/endovascular repair or antithrombotic treatment.
Arguments exist as to which treatment is best, with questionable benefit to endovascular stents due to many of the associated complications such as post-stenting stroke, stent occlusion, or procedural complications. One prominent study by Burlew et al from the Denver Health Medical Center finds that administering heparin for BCVI is an effective treatment for stroke prevention and that routine endovascular stenting provides no additional benefit, but should be reserved instead for rare symptomatic BCVI or patients with a markedly enlarging pseudoaneurysm.8 In a study of asymptomatic patients with BCVI treated with heparin infusion, stroke rate was decreased to 0.3%.9
Recommendations have been made to treat grade I-IV injuries with low-dose anticoagulation via heparin infusion. Antiplatelet agents, such as aspirin with or without clopidogrel, have also been suggested and potentially have similar efficacy in stroke prevention; however, there have not been large studies to support this currently. Many low-grade injuries (ie, Grade I and II) heal within 7-10 days, therefore early repeat CT-A is recommended to evaluate, as this may allow for discontinuation of antithrombotics at that time. Otherwise, treatment is continued typically for 3-6 months, at which point re-imaging is recommended to evaluate for resolution.5
Conclusion
BCVI is a relatively rare condition associated with significant morbidity and mortality that can be prevented if identified early. Emergency physicians are incredibly important in diagnosing this disease and must know which trauma patients require advanced imaging so they may identify BCVI early in the hospital course.
Key factors in identification involve recognizing high risk injury patterns and utilizing the appropriate screening imaging modality. With prompt diagnosis and treatment, trauma patients with BCVI may be spared from long-term neurologic disability.
References
1. Hwang PYK, Lewis PM, Balasubramani YV, Madan A, Rosenfeld JV. The epidemiology of BCVI at a single state trauma centre. Injury. 2010;41(9):929-934.
2. Biffl WL, Burlew CC, Moore EE. Blunt cerebrovascular injury: Treatment and outcomes. UpToDate.com. Published 2018.
3. Mattox KL, Moore EE, Feliciano DV. Trauma. 7th ed. Philadelphia, PA: McGraw Hill; 2012.
4. Burlew CC, Biffl WL. Blunt cerebrovascular trauma. Curr Opin Crit Care. 2010;16(6):587-595.
5. Burlew CC. Blunt Cerebrovascular Injury. Critical Care of the Surgical Patient. Decker. Published 2018.
6. Grigorian A, Kabutey NK, Schubl S, et al. Blunt cerebrovascular injury incidence, stroke-rate, and mortality with the expanded Denver criteria. Surg (United States). 2018;164(3):494-499.
7. Geddes AE, Burlew CC, Wagenaar AE, et al. Expanded screening criteria for blunt cerebrovascular injury: a bigger impact than anticipated. Am J Surg. 2016;212(6):1167-1174.
8. Burlew CC, Biffl WL, Moore EE, et al. Endovascular stenting is rarely necessary for the management of blunt cerebrovascular injuries. J Am Coll Surg. 2014;218(5):1012-1017.
9. Burlew CC, Biffl WL, Moore EE, Barnett CC, Johnson JL, Bensard DD. Blunt cerebrovascular injuries: Redefining screening criteria in the era of noninvasive diagnosis. J Trauma Acute Care Surg. 2012;72(2):330-337.