Quick recognition of the Bezold-Jarisch reflex triad of hypotension, bradycardia, and apnea is important for any physician who administers nitroglycerin. This knowledge can ensure positive patient outcomes and avoid cardiopulmonary collapse.
Case Presentation
A 59-year-old male presented to the emergency department through the lobby with general malaise, dizziness, and hypertension for 6 days prior. In triage, the patient endorsed acute subtle chest pressure with no associated pain or radiation. Patient denied shortness of breath, nausea, abdominal pain, jaw pain, arm pain, or headache. No pertinent family or past medical history was reported.
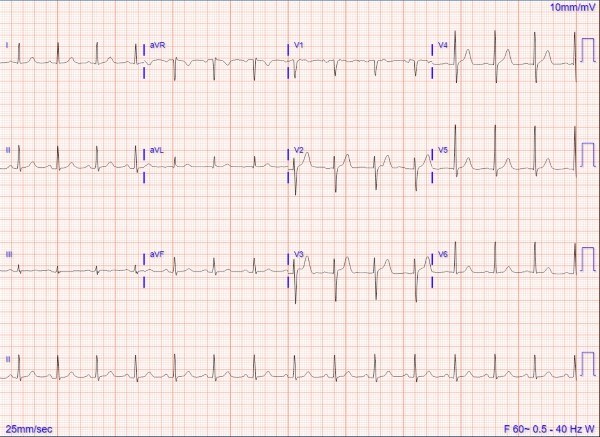
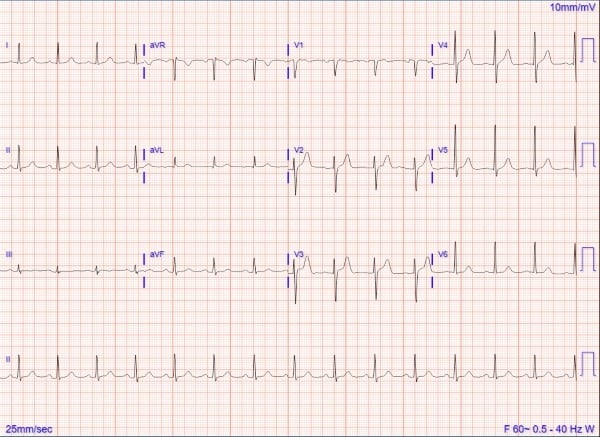
An initial EKG showed normal sinus rhythm at 87 bpm with no ST-segment or T-wave abnormalities. Initial vital signs were notable for a BP of 208/114 with no other abnormalities. Cardiac exam showed normal rate and rhythm, with no murmur heard. No known drug allergies were confirmed with the patient.
The initial treatment modalities for hypertension and chest pain included 0.4 mg sublingual nitroglycerin and 324 mg chewable aspirin. Five minutes after medication administration, the patient became unresponsive and diaphoretic, with pulse in the 20s and a blood pressure of 50/30s. The patient became unresponsive to painful stimulus, with no palpable carotid pulse, and CPR was initiated. The patient immediately woke up with initiation of CPR but was lethargic, with a weak carotid pulse in 30s.
Further treatment with 1mg atropine IV and a normal saline bolus was started. Shortly after, the patient’s pulse improved to 80s and the blood pressure improved to 80s/60s. The patient fully returned to baseline mental status 5 minutes after atropine administration, with no pertinent findings on repeat exam.
Labs showed hyponatremia at 126 mmol/L, negative BNP, and high-sensitivity troponin of 22ng/L with repeat delta troponin at 20 ng/L. The patient was admitted for continued monitoring. Echocardiogram showed normal systolic function with normal LVEF 65%, no wall motion abnormalities, and no valvular abnormalities. No further cardiac events were observed, and serial troponin markers remained negative. A work-up for acute coronary syndrome (ACS) was negative.
Cardiology was consulted and noted that the initial reaction was likely Bezold-Jarisch reflex. The patient’s presenting symptoms were attributed to poorly controlled hypertension. His medications were adjusted, and he was ultimately discharged in stable condition.
Discussion
The case underscores the clinical significance of the Bezold-Jarisch reflex (BJR). Pertinent chart reviews and case studies revealed few clinically relevant cases involving nitroglycerin induced BJR. In prior cases where Bezold-Jarisch reflex was observed, those patients typically had underlying cardiac pathology.2,3 The BJR has rarely been documented in patients who have a non-cardiac etiology of their symptoms or have no prior cardiac history.
This case demonstrates that Bezold-Jarisch reflex can be seen in patients without underlying cardiac pathology. Given the prevalence of nitroglycerin administration in the ED, it is important for physicians to recognize this as a medication side effect. Quick recognition of the Bezold-Jarisch reflex triad of hypotension, bradycardia, and apnea is important post administration of nitroglycerin to ensure positive patient outcomes and avoid cardiopulmonary collapse.
In this case, the patient’s bradycardia was effectively treated with atropine and their hypotension was managed with fluid resuscitation. While research on this reflex is minimal due to the isolated nature of this reaction, it warrants consideration in patients showing unexplained apnea, hypotension, and bradycardia. The management above, atropine and IV fluid resuscitation, may be considered if this reaction is witnessed.
TAKE-HOME POINT
It remains crucially important for physicians to maintain vigilance for a rare but life-threatening reaction that can occur from a frequently utilized medication.
References
- Akbar H, Foth C, Kahloon RA, et al. Acute ST-Elevation Myocardial Infarction. [Updated 2023 Jul 31]. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.
- Come PC, Pitt B. Nitroglycerin-induced severe hypotension and bradycardia in patients with acute myocardial infarction. Circulation. 1976 Oct;54(4):624-628.
- Shah SP, Waxman S. Two cases of Bezold-Jarisch reflex induced by intra-arterial nitroglycerin in critical left main coronary artery stenosis. Tex Heart Inst J. 2013;40(4):484-486.