Emergency medicine features heavily in recent media reports regarding “surprise” medical bills.1,2 Whether questioning the utility of emergency care, the associated hospital fees, or the changes in insurance coverage, most of these reports fail to recognize emergency medicine’s unique position at the intersection of the failures of access, coverage, and payment in the modern health system.
Our specialty is more frequently being put in a defensive position by patients, media, and the government. Though many factors contributing to the issue are out of our hands, the current policy landscape lends us some control to help our patients and our specialty.
WHAT IS BALANCE BILLING?
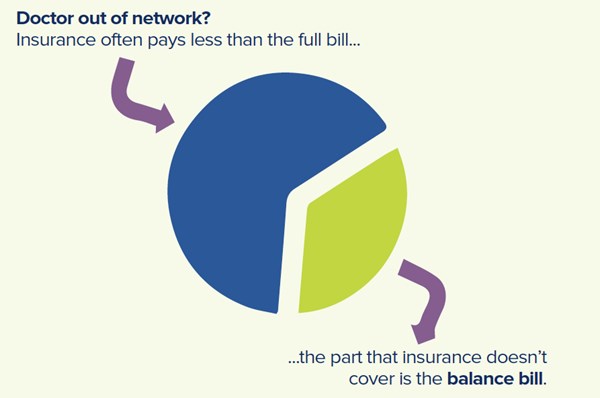
A medical emergency can often be one of the most frightening moments of a person’s life. When faced with a problem like uncontrolled bleeding, chest pain, or a stroke, patients often seek treatment from the nearest emergency department. After a patient has been treated and stabilized, their physician then bills an insured patient’s health insurance company. If the provider is “in network,” meaning they have a pre-existing contract to provide medical services at a specific rate, the insurance company provides the full negotiated reimbursement. If the provider and health insurance company do not have a contract, the services are “out of network” (OON), and insurance companies often pay a lower rate. The physician who provided the required emergency care may then try to recover the unpaid balance – the difference between the lower out-of-network rate and the standardized payment for that service – by billing the patient for the difference. This practice is known as balance billing.
When patients do not understand their insurance coverage and the implications of OON care, they can be caught off guard by these balance bills. Further complicating the matter is the increasing prevalence of other cost-raising changes to insurance coverage. In particular, high-deductible insurance plans increase out-of-pocket costs for patients in the form of rising deductibles and copays. All of these changes – balance bills, high deductibles, and increased copays – are often lumped together in the popular media and labeled as “surprise bills”.3,4 What patients often view as “surprise bills” are actually the result of insurance companies narrowing their networks and increasing costs to patients.
BALANCE BILLING CAN AFFECT ANYONE
Balance billing burdens all medical specialties, but emergency care is the only care required by law to be provided regardless of insurance status as delineated by the Emergency Medical Treatment and Labor Act (EMTALA).5 Further, when patients are having a medical emergency, they often do not get the chance to figure out which emergency physicians are in network or out of network. As would be expected, emergency medicine accounts for about one-quarter of cases of balance billing.6 While the percentage is not insignificant, the prevalence of balance billing may actually be as low as 2% of ED bills.7
BALANCE BILLING IN EMERGENCY MEDICINE
Emergency physicians serve an important role in the health care system by acting as the health care safety net for patients regardless of their insurance status. Physicians may agree to accept a lower in-network rate for their services in exchange for an easy, streamlined reimbursement process and higher patient volumes. Health insurance companies benefit from this arrangement, as evidenced by their reporting of record profits and stock increases.8 When a health insurance company tries to further increase profits by refusing to contract for a fair amount, any care provided by that physician is reimbursed at an OON rate, leaving a large balance that is the responsibility of the patient.
A FURTHER COMPLICATION
The relationship between hospitals and the physicians that staff them adds an additional layer of complexity to the matter. While hospitals may opt to negotiate with health insurance companies to create in-network contracts, emergency departments are often staffed by physicians from independent companies. Naturally, these physicians often want to protect their right to independently negotiate with health insurance companies before entering into contracts, and patients may not realize that their in-network hospital may be staffed with OON physicians. Though the prevalence of this discordance is not known nationally, a recent study in Texas showed that at least some insurers offered no in-network emergency physicians at more than half of their in-network hospitals.9 Both physicians and patients suffer when insurance companies refuse to provide reasonable options.
POLICY SOLUTIONS
Patients reasonably expect their health insurance to cover their emergency care. Balance billing pits patients and physicians against each other. As expected, consumer advocacy groups and federal and state legislatures are stepping up to find solutions.10 Proposed solutions include required reimbursements, balance billing limits, and advance disclosure requirements. Some of these policies have found a home in federal and state laws over the last decade, closing some of the gaps, but leaving the need for a more comprehensive solution.11 In January 2019, ACEP presented a framework to curb the rise of these bills.12
REQUIRE REIMBURSEMENT
Health insurance companies have the right to reimburse OON physicians at a lower rate than their in-network colleagues.13 Recognizing this disparity, the Affordable Care Act (ACA) levels the playing field by requiring some health insurance companies to reimburse at only the in-network rate.14 Required reimbursement rates reduce the amount of balance billing, but the solution has several flaws. First, the ACA only makes changes to new and federally regulated health insurance plans. It does not require the in-network reimbursement rate for grandfathered plans nor for self-funded, employer-sponsored plans, which make up the majority of health insurance in the US. Second, in-network rates may be unreasonably low. This is evidenced by the fact that some OON physicians have chosen not to accept the lower rates offered by in-network contracts with the health insurance company in the first place.15 Any balance left between the physician’s rate and the reimbursed rate is still subject to balance billing, and the ACA provides no provision to address that.
LIMIT BALANCE BILL AMOUNTS
Another solution proposes legal regulations to prohibit or limit the amount of the balance bill, which provides a certain amount of protection to patients. States like Texas and New York pioneered this policy solution of limiting balance billing. As with the policy requiring reimbursements, this solution is not without flaws. For many patients, the balance bill limit ($500 in Texas, for example) is not an insignificant expense. At the same time, the actual bill may be substantially higher, leaving the physicians who are legally required to provide medical care without a legal guarantee to payment for that care. Appeals are possible; Texas provides for a mediation process for higher bills, and New York provides for a binding arbitration process.16, 17 As with the aforementioned required reimbursements, these policies apply differently to different types of insurance, leaving many patients and physicians without a solution.
REQUIRE ADVANCE DISCLOSURE
Some states require disclosure in advance so that a patient can make an informed decision about whether to accept out-of-network care.18 This solution makes sense for non-emergent care when there is time to research in-network physician options. In medical emergencies, the luxury of time rarely exists, meaning advanced disclosure is of limited value.19Requiring insurers to disclose deductibles on their insurance cards would also help inform patients of their responsibility when seeking medical care.
FORCE IN-NETWORK CONTRACTS
One way to reduce the burden on patients for identifying in-network providers can be found in the private sector. In an effort to reduce the number of in-network hospitals staffed by out-of-network physicians, some hospitals have begun requiring all physicians to enter into in-network contracts with health insurance companies.20 Private sector solutions often benefit hospitals and insurance companies. Physicians are often harmed as they face a difficult negotiating position and reduced employment prospects.
HOW YOU CAN HELP
As patients, physicians, and insurance companies work to reduce the amount of balance billing, the policies surrounding the issue continue to evolve. Earlier this year, President Trump stated his support for banning these sorts of bills.21 The Senate is also pushing a bipartisan solution.22 No current government solution fully recognizes emergency physicians’ unique vantage point on this matter. Emergency physicians have an ethical and legal obligation to treat all patients, and their engagement in the conversation regarding solutions is more vital than ever. Emergency physicians who do not advocate for their position risk losing their voice regarding future regulations. Continuing to communicate the opportunities inherent in serving as the health care safety net, coupled with the burdens of the unfunded mandate of EMTALA, will help guide future government regulations and private sector actions that will most benefit patients.
References
- Kiff, S. After Vox story, Zuckerberg hospital promises to change its aggressive billing tactics. Vox. 1 Feb 2019.
- Galewitz, P. A Fainting Spell After A Flu Shot Leads To $4,692 ER Visit. NPR. 28 Jan 2019.
- Radnofsky L, Armour, S. States Start to Approve Steep Increases in Health Premiums. The Wall Street Journal. 24 Aug 2016.
- Consumerist: Insurance Loopholes & Master Pricing: How Surprise Medical Bills Knock Consumers Down. Consumer Reports. 24 Sept 2015.
- 42 U.S.C. § 1395dd
- Kyanko, K, et al. Out‐of‐Network Physicians: How Prevalent Are Involuntary Use and Cost Transparency? Health Services Research. 22 Oct 2012
- Berry, K. Reference-Based Pricing is Being Redefined. Benefits Magazine. Vol 52, No 10, Oct 2015.
- TDI Fines Humana Over Network Adequacy. Texas Department of Insurance. 8 Oct 2018.
- Sommer, J. Gripes About Obamacare Aside, Health Insurers Are in a Profit Spiral. The New York Times. 18 Mar 2017.
- Meet Physicians for Fair Coverage. Physicians for Fair Coverage. Accessed 4 Aug 2018.
- Murphy, B. 20 things to know about balance billing. Becker’s Hospital Review. 27 Jan 2017.
- ACEP Presents Framework To Protect Emergency Patients From Out-Of-Network Billing Issues. ACEP. 28 Jan 2019.
- See Federal Register, Jun 28, 2010, pp. 31788-37421.
- The Patient Protection and Affordable Care Act (PPACA), Pub. L. No. 111-148, 124. Stat. 119. 23 Mar 2010.
- Carroll, J. The Ingenix Aftermath. Managed Care. 1 May 2009.
- Herman, B. Billing squeeze: Hospitals in middle as insurers and doctors battle over out-of-network charges. Modern Healthcare. 29 Aug 2015.
- Surprise Medical Bills. Texas Department of Insurance. Accessed 4 Aug 2018.
- Hoadley J, Ahn S, and Lucia K. Balance Billing: How Are States Protecting Consumers from Unexpected Charges? Georgetown University Health Policy Institute. Jun 2015.
- A Resource for Emergency Physicians on Balance Billing, Out-of-Network Fees, and Surprise Bills from The Independent Practice Support Committee of the American Academy of Emergency Medicine. AAEM. Accessed 29 Nov 2018.
- Bannow, T. Hospitals' solution to surprise out-of-network bills: Make physicians go in-network. Modern Healthcare. 12 Jan 2019.
- Sullivan, P. Trump calls for cracking down on surprise medical bills. The Hill. 23 Jan 2019.
- Adler, L. et al. Analyzing New Bipartisan Federal Legislation Limiting Surprise Medical Bills. Health Affairs. 25 Sept 2018.