Obtaining arterial access is a common procedure in both emergency medicine and in critical care.
We as residents do these countless times in resuscitation bays and intensive care units and will continue to perform them into our attending years. In fact, it is estimated that 8 million arterial catheters are placed in the United States each year.1
One of the most common reasons for arterial line placement is for accurate and precise monitoring of blood pressure; often used to titrate vasopressors to target a mean arterial pressure for organ perfusion. Septic shock is one of the most common causes of shock and a leading cause of mortality and critical illness in the ED and in the ICU.2 The radial artery is by far the most common site for arterial lines but there can be various reasons why this site might not be an appropriate choice.3 Common reasons being: arterial thrombus from prior arterial lines (a complication in 20%-35% of radial catheters), significant vasoconstriction/vasospasm from prior catheterization attempts or from high pressor requirements, and local infection as well.4When another location is needed, most often the femoral artery is then chosen.3 What if this location is also not available? The femoral location might be a poor choice due to similar contraindications above or due to additional issues specific to its location such as body habitus/large pannus, stool/urine incontinence, aortoiliac surgery/stent history, etc.5
Here we will discuss the axillary artery as an alternative location for placement of arterial catheters for hemodynamic monitoring, frequent lab draws, etc.
There are many theoretical benefits to the axillary artery as a location for arterial catheterization - one being that when compared to the radial site, the axillary artery has the benefit of possibly more closely reflecting central perfusion pressures due to its more proximal location. Given our express goal is often to maintain perfusion to central organs, this can clearly be desirable. In fact, there have been numerous studies of patients with shock physiology that have looked to see if there is a difference in measured pressures when comparing distal to central sites of arterial blood pressure monitoring. Although these studies almost exclusively feature radial versus femoral artery comparisons, many of them do demonstrate lower mean arterial pressures when radial catheters are used—average differences of 4-15mmHg in mean arterial pressures.6-8 The 2013 Kim paper even demonstrated a dose-like relationship in which this difference narrowed as vasopressors were weaned.8 Together this suggests the possibility that axillary catheters (being larger and in a more central location like femoral lines) may allow for more accurate monitoring of central organ perfusion pressures and allow for lower doses and earlier discontinuation of vasopressors leading to less risk of side effects associated with vasopressors.
The actual setup and technique of placing an axillary arterial line share a lot of similarities to radial and femoral site approaches, so you will already have many of the skills needed for learning this procedure. You will need to collect the same supplies you would for a femoral approach, with the only addition being a soft upper extremity restraint to help with patient positioning. This means you will need your PPE, probe cover, skin site prep, fenestrated drape, topical anesthetic supplies, and a femoral catheter kit complete with: needle, wire, scalpel, catheter, suture, a prepared arterial line connection set-up, and sterile occlusive dressing.
Figure 1. Arterial line kit contents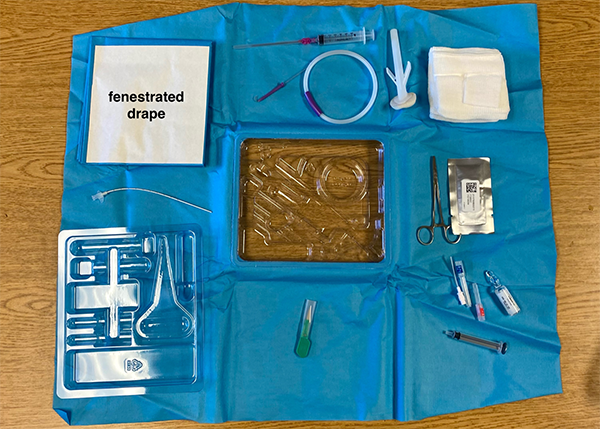
Patient Positioning
Place the extremity in an abducted and externally rotated position with the upper arm at 90-135° abducted from the chest wall and the palm facing toward the ceiling and above the patient's head. This will open the axilla, which can then be sterilely prepared and draped—body hair may need to be removed to accomplish this.
Figure 2. Appropriate patient positioning
Technique
Using a high-frequency linear probe optimized for near-to-mid field resolution, find the third portion of the axillary artery. Useful landmarks on exam to locate this third portion include the inferior border of the pectoralis minor, which marks the start of the third segment of the axillary artery, and the inferior border of teres major, which marks the end of the axillary artery itself and the start of the brachial artery.
Figure 3. Ultrasound anatomy of axilla. PM=pectoralis minor, AA=axillary artery, AV=axillary vein, NC=nerve cords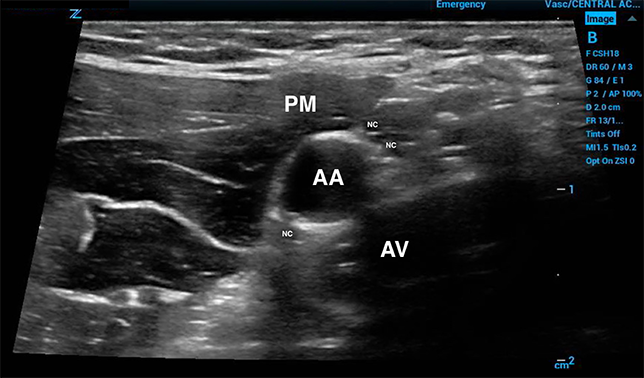
This location is ideal, as it preserves collateral blood supply but also approaches the artery distal to the dense collection of the brachial plexus nerve cords. Care should be taken to scan for any nearby nerves or vessels so these can be avoided and used to search for the appropriate anatomic site. From there use the same Seldinger technique used for femoral artery access, finally directing the catheter over the wire into the axillary artery towards the patient's core (do not place the catheter toward the patient's hand).
Troubleshooting and Mistakes to Avoid
Use an appropriate catheter (typically a stiffer femoral artery line kit) and not radial artery catheters which will be too short. Preloaded femoral artery catheters may have thinner walls and might be more prone to kinking.
Figure 4. Close-up of femoral (axillary) catheter with syringe for scale
Flush axillary artery catheters slowly to eliminate the theoretical risk of pushing air embolisms into carotid arteries. The large case series reviewed for this post does not report any such theoretical events despite thousands of recorded procedures.
The axillary artery does closely abut the brachial plexus and the nerves that extend from this plexus—any developing paresthesias in the ipsilateral limb of the procedure should be taken seriously. Routine monitoring for hematoma and neurovascular checks of the distal extremity should be included in the post-procedure care plan, and developing hematomas should be managed with direct pressure and removal of the line if needed.
Given the large caliber of the vessel, any failed attempts should be monitored for developing hematomas and pressure should be held at the site of any failed attempt for multiple minutes and/or until bleeding stops.
The axilla is dense in sweat glands and therefore may require more frequent dressing changes when compared to the other common arterial line sites.
Conclusion
Axillary artery cannulation should be done only by experienced clinicians or under the direct and close supervision of such a clinician.
The procedure has been done numerous times in published literature and described in a handful of other locations but much of the procedure, its risks, its benefits, etc., is extrapolated from the more commonly done femoral site access.
When options are limited, the axillary artery poses another anatomic location for arterial catheter placement.
References
- Gardner RM. Direct arterial pressure monitoring. Curr Anaesth Crit Care. 1990;1(4):239-246.
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–810.
- Scheer B, Perel A, Pfeiffer UJ. Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care. 2002;6(3):199-204.
- Wallace MW, Solano JJ. Radial Artery Cannulation. [Updated 2021 Jul 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021.
- Htet N, Vaughn J, Adigopula S, Hennessey E, Mihm F. Needle-guided ultrasound technique for axillary artery catheter placement in critically ill patients: A case series and technique description. J Crit Care. 2017;41:194-197.
- Dorman T, Breslow MJ, Lipsett PA, et al. Radial artery pressure monitoring underestimates central arterial pressure during vasopressor therapy in critically ill surgical patients. Crit Care Med. 1998;26(10):1646–1649.
- Galluccio ST, Chapman MJ, Finnis ME. Femoral-radial arterial pressure gradients in critically ill patients. Crit Care Resusc. 2009;11(1):34–38.
- Kim WY, Jun JH, Huh JW, Hong SB, Lim CM, Koh Y. Radial to femoral arterial blood pressure differences in septic shock patients receiving high-dose norepinephrine therapy. Shock. 2013;40(6):527–531.



