If you practice in a state where Anthem operates, you might be seeing fewer patients, sicker patients, or those who come to you too late for meaningful help - because their insurance company has begun denying claims retroactively if a condition turns out not to have been emergent. ACEP has sued to stop this dangerous practice. What can you do to protect patients?
A key selling point for health insurance is peace of mind. People pay monthly premiums for those moments when they develop a strange rash or a sudden tightening in their chest. So imagine their shock upon receiving a letter from their insurer stating, “Save the ER for emergencies. Or you’ll be responsible for the cost.”1 In January, Anthem expanded their rollout of such letters to policyholders in 14 states. Based on retrospective claim reviews, the nation’s largest insurer is retroactively determining if the patient’s case was emergent or not. Lawmakers, physicians, and patients have complained about both the detrimental health effects and dubious legality of this policy. Anthem asserts it intends to reduce wasteful health care spending – but its approach highlights the need for transparency in the industry.
Rather than working with providers to provide a sustainable long-term solution in the form of coordinated care between primary care physicians and hospitals, Anthem hopes to intimidate patients into filing fewer claims. Jeremy Faust, MD, MS, attending physician at Brigham and Women's Hospital/Harvard Medical School, is dismayed by Anthem’s approach.
"It takes medical students and residents years of training and thousands upon thousands of patient encounters to learn to identify which patients are truly having an emergency and which are not,” Dr. Faust said. “Asking patients to play doctor based on symptoms alone is unrealistic and frankly dangerous. The reality is that patients have no idea whether their symptoms are serious or not.
“In fact, a great deal of physicians have no idea whether patients are having a true emergency or not. That's why emergency medicine as a field exists."
Anthem argues that all billing codes related to a visit were reviewed by a physician. Aside from this review coming after the fact, the Missouri Hospital Association reviewed a previous list of codes Anthem had deemed avoidable ED usages and found that only 15% of the 1,900+ codes were considered truly avoidable by the widely cited NYU ED code database.1 In fact, only 5% were considered always non-emergent. No patient should ever worry if a severe allergic reaction or an automotive accident deserves emergent care or not. Yet reporters have documented Anthem’s initial rejection of claims related to each of these situations.1-2 While Anthem maintains its current list has been updated, it has never provided a copy of this new list.
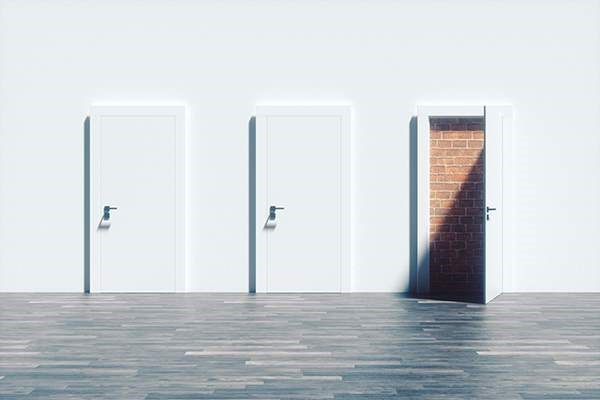
Imagine a customer purchasing a warranty for their phone that voided based on certain conditions, but then being told they couldn’t read the fine print - and that after they elect for a repair, a technician will arbitrarily accept or deny coverage. Anthem refuses to release its updated list of non-emergent codes and/or codes it would consider potentially non-emergent. Anthem essentially tells their members, “Your policy has potentially budget-crushing fine print, but no one gets to read it. In fact, we’ll determine if you are ineligible after you are already on the hook.” In many states, these lists remain confidential, despite lawmakers’ requests. No health care spending solution should be premised on the utter lack of transparency from the party responsible for settling the bills.
Trevor Pour, MD, FACEP, attending physician at Mount Sinai Hospital/Icahn School of Medicine, points out the egregious financial implications. “We often refer to the ED as a ‘safety net’ for good reason; we see patients regardless of their ability to pay,” Dr. Pour said. “But if a visit comes with the risk of a 4-figure price tag, it's suddenly out of reach for most Americans.”
Without a publicized and responsibly chosen list of non-emergent codes, Anthem’s policy will continue to intimidate patients into second-guessing their medical emergencies. Dr. Pour worries the policy rolls back decades of hard work by physicians and hospitals to save lives. “For years, the American Heart Association (AHA) and others have waged public health campaigns urging patients to call 911 with symptoms of strokes and cardiac events. But now we've got a policy that potentially punishes patients for following those instructions, if their eventual diagnosis turns out to be reflux, costochondritis, or a tension headache.”
Echoing his and others’ concerns, the head of the AHA pointed out in a 2016 letter to Missouri physicians and hospitals, “The very real unintended consequence of such a policy is to discourage their policyholders from immediately seeking or altogether foregoing potentially life-saving care when time is of the essence.”3
Dr. Faust can easily imagine such a scenario. “I remember a patient who was sent to the emergency department with chest burning. She was convinced it was acid reflux, but what she had was a massive ST-elevation myocardial infarction,” he said. “Imagine if she had sat at home thinking to herself: ‘I better not go to the hospital because this is probably not a real emergency and I'm going to get a huge bill when my claim is rejected.’”
After lawmakers like Sen. Claire McCaskill, D-MO, threatened to bring legislative pressure through the Affordable Care Act’s prudent layperson standard (which states insurers must reimburse must cover ED visits that “a prudent layperson who possesses an average knowledge of health and medicine” determined necessary), Anthem made concessions in February to always cover visits involving surgery, IV fluids, MRI/CT scans, or if billed as urgent care.4 In addition, Anthem claims that medical records will be requested along with billing codes. As ACEP has pointed out, these concessions do not change the fact that patients are being asked to make in-the-moment determinations of symptom severity with the possibility of crippling financial bills hanging over their heads.5
While the prudent layperson standard will continue to be litigated by interest groups, the lack of informed discussion and accountability about what constitutes non-emergent care is a huge part of the problem. In addition to requiring medical record review by physicians, the industry must be willing to provide their diagnosis code lists – the terms and conditions of the warranty. There may be a reasonable case for withholding reimbursement for a limited number of codes that would be clearly non-emergent to the average patient. But that list must be made public for providers and watchdogs to examine and debate. Economists have always admitted that health care is a singularly essential good for a consumer: drop a smartphone in the ocean and life goes on; brush off a tightening chest and life could be over.
Efforts to reduce utilization should and must be pursued, but not at the expense of the patient (both his pocketbook and his life). For Dr. Pour, gambling with patients’ lives to avoid potential abuse is untenable. “Of course, every emergency physician has seen their share of ED abuse; I had a patient last week who earnestly said they were hungry and needed a sandwich – and this was their only complaint,” Dr. Pour said. “But I'm happy to keep my doors open for dozens of those visits if it means we're not missing the true emergency – a heart attack, stroke, or worsening infection or surgical emergency – who is deteriorating at home over fear of cost.”
ACEP Sues Anthem to Protect Patients
ACEP and the Medical Association of Georgia sued Anthem s Blue Cross Blue Shield of Georgia in July, asking a federal court to halt Anthem's retroactive denials of emergency care. The lawsuit asserts that Anthem's policy — which is being used in Georgia and 5 other states — violates the prudent layperson standard and also violates the 1964 Civil Rights Act because Anthem's denials disproportionately affect members of protected classes.
“We can’t possibly expect people with no medical expertise to know the difference between something minor or something life-threatening, such as an ovarian cyst versus a burst appendix,” said ACEP President Paul Kivela, MD, FACEP. “ACEP and MAG have tried multiple times to work with Anthem to express these concerns and urge them to reverse this policy, and they have refused. We felt we had no choice but to take action to protect our patients, and therefore are asking the federal court to force Anthem's BCBS of Georgia to abide by the law and fulfill their obligation to their policyholders."
What Can You Do Now?
Get involved in the Fair Coverage fight. Visit www.faircoverage.org for details.
Jeremy Faust, MD, MS
"I'm concerned that the prudent layperson policy punishes people with poor health literacy and has discrimination against those with cognitive disabilities baked right into it. The standard based on an ‘average knowledge of health and medicine’ sounds reasonable until you remember that half of all people have below-average knowledge of health and medicine. Many of our patients, including those with substantial cognitive impairments, don't have the luxury of being able to assess their own risks. Is Anthem going to punish them for that?"
Trevor Pour MD
"Just recently, I cared for a young woman who delayed an ED visit for worsening ulcerative colitis due to her concerns about her co-pay. By the time she arrived, her condition had significantly worsened. We need to reduce the barriers to seeking timely care, not expand them.”
On the problem with asking patients to determine the true urgency of their condition
"We're able to use our years of medical training, along with a good physical exam, to determine whether a patient's complaint needs immediate testing and/or treatment. Yet even with those tools, we frequently need EKGs, imaging test, and labs to judge if a condition is emergent. But most patients aren't armed with that knowledge and depend on us to help them. Putting the onus on the patient, who has no medical training and no access to those resources, is misguided and dangerous."
References
1. Murphy T, Associated Press. Is it an emergency? Insurer Anthem makes patients question ER visits. Star Tribune. Published Nov. 30, 2017. Accessed May 25, 2018.
2. Livingston S. Anthem’s new ED policy leaves patients reeling from large medical bills and hospitals buried under claim denials. Modern Healthcare. Published Dec. 2, 2017. Accessed May 25, 2018.
3. Brown N. Anthem Policy Change. American Heart Association. Published Nov. 6, 2017. Accessed May 25, 2018.
4. McCaskill, C. Letter to Joseph R. Swedish. Office of Sen. Claire McCaskill.Published December 20, 2017. Accessed May 25, 2018.
5. Wooster L. ACEP Battles Anthem BlueCross BlueShield Policy That Jeopardizes Prudent Layperson Standard. ACEP Now. Published March 14, 2018. Accessed May 25, 2018.