By sharing EM knowledge internationally, we can integrate new and effective methods of delivering emergency care domestically.
Background
Thanks to an EMRA-sponsored Global Health Initiative scholarship, I recently had the opportunity to travel to the U.K. and rotate through Queen Elizabeth Hospital Birmingham's Accident and Emergency Department. Coming from Washington University in St. Louis, I was uncertain what to expect. I didn't know if the population would be the same, or if practice patterns would be similar — what was it going to be like working in such a different health care system? Would emergency medicine be the same? What lessons would I learn?
There are certainly a number of similarities in emergency care between our two countries, but a number of striking differences are also readily apparent. I worked in Queen Elizabeth Hospital (QE), a large, academic tertiary care facility. It is also a major trauma referral center, and has an annual ED census approaching 100,000 patient visits per year. It is demographically comparable to many of the training institutions that residents staff in the United States, and in a similar city practice environment. In our constantly changing health care climate, I found juxtaposing our two systems enlightening.
A useful comparison
According to the World Bank, from 2009-2013 the United States spent 17.9% of its gross domestic product (GDP) on health care.1 In comparison, the United Kingdom spent only 9.3% of its GDP on health care during the same period.1 Yet despite our increased spending, the U.S. consistently ranks below the U.K. and other First World countries in health care system performance measures, including quality, access, efficacy, and equity of care.2,3 In the most recent international health care rankings by the commonwealth fund, the U.K. ranked second overall behind the Netherlands.2 In this era of health care reform, it is worth investigating the different ways in which EM is effectively practiced in other countries with similar financial and technological resources.
The National Health Service: A brief history
The U.K. established the National Health Service (NHS) in 1954. The NHS is a universal health care system, and its central principle is that health care should be freely available to all its citizens. While the NHS has been widely supported by the public, in the 1990s it was hampered by insufficient numbers of physicians and nurses, inadequate hospital equipment, and a lack of national standards. EDs were particularly affected, plagued by long wait times and a lack of integration within the greater health care system.4 In 2000, in response to these issues, then Prime Minister Tony Blair enacted a major overhaul of the NHS.
The four-hour target
The introduction of the “four-hour target” was perhaps one of the most dramatic outcomes of the 2000 NHS plan. Under this guideline, hospitals were given major financial incentives to update and streamline emergency care with the final goal of all emergency care not exceeding four hours in total.4 This four-hour clock starts from the moment the patient checks into the ED, and ends when the patient is physically out of the ED. With the implementation of this rule, by 2006 over 95% of patients in a crosssection of 20 EDs across England were seen and treated within 4 hours.5
In 2013, QE and my home institution were evenly matched with 96,167 patient visits and a 28% admit rate, and 95,600 patient visits and a 27% admit rate, respectively. QE, however, was able to meet its patient load with one-third of the ED bed space — an achievement made possible, in large part, by the non-existence of ED boarding.
That said, controversy remains regarding whether meeting this four-hour target actually improves patient outcomes.6 It must also be noted that there are significant differences in medical landscapes between the U.S. and the U.K., and the potential impact of legal action against ED physicians in the U.S. cannot be ignored. In a similar vein, many aspects of the four-hour rule are contrary to basic standards of ED care in the U.S. For example, in the U.K., the admitting providers —not the ED team — follow up all non point-of-care ED labs, including troponins in non-STEMI chest pain; and patients never stay for a second troponin in the ED (although they may be admitted for additional testing).
With the current climate of bed shortages, nursing shortages, and ED and hospital overcrowding, a four-hour target is unlikely to be successful in most academic institutions in the U.S. However, as ED wait times grow and physician performance is increasingly evaluated based on patient satisfaction, concrete time endpoints to ED visits may be needed. Any target time should have buy-in from the hospital administration and should allow sufficient time to accomplish initial resuscitation, diagnostic and laboratory testing, and preliminary interventions, while also decreasing ED overcrowding and improving patient satisfaction.
EM training
Emergency medicine training has been available in the U.K. since 1972, and has been a board-recognized specialty since 1983.7 Compared to the now streamlined EM training scheme in the States, training in the U.K. is more protracted (Table 1). Training sites at the “foundation” and “basic” training levels are randomly selected and do not always include EM rotations, which makes it challenging for future U.K. physicians to gain exposure to the specialty. Additionally, not all EM registrar (residency) programs include training at a regional trauma center (level I trauma center), which can lead to deficiencies in the knowledge of ED trauma management.
ED staffing and supervision
At this time, all attending-level physicians in the NHS across all specialties are paid approximately £48,000 per year and work approximately 48 hours per week. This has made it difficult to recruit new physicians into EM, as many choose to become general practitioners with the associated regular weekday schedule without night or weekend responsibilities. At QE, there are only 11 EM board-certified attendings and eight EM registrars to cover the hospital's volume of nearly 100,000 patient visits per year. In comparison, my home institution in St. Louis has 47 EM attendings and 48 EM residents to cover the same patient load. As a result, many U.K. EDs are staffed primarily by physicians in their foundation and basic training years, even at major academic level I trauma centers like QE. Many EDs are never staffed with an attending, and the attendings provide only home call coverage at night. In the U.S., on the other hand, my EM attendings still staff every patient who comes through the ED.
MERIT: Medical Emergency Response Intervention Team
Another difference between the NHS and U.S. systems is the MERIT pre-hospital crew. Within the West Midlands Regional Trauma Network, which services most of the middle and western parts of England and Wales, there is a 24/7 MERIT team composed of one EM or critical care-trained physician, and one trauma-critical care paramedic. They respond via helicopter by day and via well-outfitted minivan by night to all level 1 traumas in the area to provide additional medical support to the on-scene paramedic team. The MERIT team was created in response to historically poor trauma outcomes in this area of the country. With assistance from the highly trained MERIT team, pre-hospital teams are more likely to effectively preform potentially life-saving pre-hospital procedures like intubation and thoracotomy. MERIT's medical expertise is so well trusted that, on arrival to a trauma center ED, stabilized level 1 trauma patients will frequently go directly to CT (before a primary or secondary survey is preformed!). Although the MERIT team is relatively new, and full outcome data on its efficacy is still pending, at this time the hospital ED and trauma teams are very pleased with this new system.
Conclusions
EM is a relatively young specialty worldwide. Systems that work well in one country can be challenging in others with different approaches to health care. However, emergency care in the U.S. would benefit from lessons learned in the U.K. regarding improved patient flow through the ED and incorporation of pre-hospital systems like the MERIT team. Conversely, if EM training in the U.K. were to become more streamlined — similar to training in the States — it might be easier to recruit physicians into emergency medicine. By sharing EM knowledge and experiences among physicians internationally, we have the opportunity to integrate new and effective methods of delivering emergency care domestically.
Table 1. Comparison of EM Training in U.S. vs. U.K.
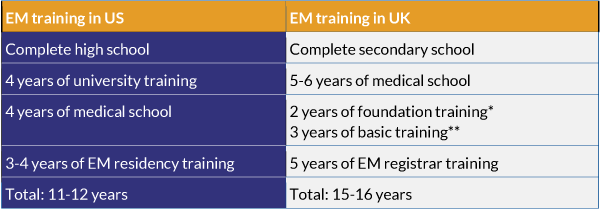 *similar to year 3-4 of medical school in the US
*similar to year 3-4 of medical school in the US
**similar to general medical or surgical internship in US
References
- The World Bank: Health Expenditure. Available from: http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS.
- Karen Davis, P.D., Cathy Schoen, M.S., and Kristof Stremikis, M.P.P. , Mirror, Mirror on the Wall: How the Performance of the U.S. Health Care System Compares Internationally, 2010 Update. 2010, The Commonwealth Fund.
- Tanne, J.H., US comes last in international comparison of health systems. BMJ, 2007. 334(7603): p. 1078
- Letham, K. and A. Gray, The four-hour target in the NHS emergency departments: a critical comment. Emergencias, 2012. 24: p. 69-72.
- Suzanne Mason, M., FRCS, et al., Time Patients Spend in the Emergency Department: England's4-Hour Rule—A Case of Hitting the Target but Missing the Point? Annals of Emergency Medicine, 2011. 59(5): p. 341-149.
- Bevan, G. and C. Hood, Have Targets Improved Performance In The English Nhs? British Medical Journal, 2006. 332(7538): p. 419-422.
- College of Emergency Medicine, Landmarks in the Development of the Specialty.



