Working in a busy ski clinic brings a variety of sports medicine injuries into focus. When your patient is a downhill skier, knee injuries are the most common injury you'll see.
A 29-year-old female is brought in by ski patrol to ski clinic. She recalls that her left knee twisted awkwardly when she fell slowly while skiing. She tells you that she felt a ‘pop’ and then immediate pain, which quickly subsided. When she attempted to ski down, her left knee felt too unstable to bear weight and she was brought in by ski patrol in a rigid knee brace.
If you work in a busy ski clinic, you will realize the scenario above is not infrequent. Knee injuries are the most common injury in skiers, in stark contrast to snowboarders, in whom upper limb injuries are more common.1 Downhill skiing has a strong association with anterior cruciate ligament (ACL) injury, with an incidence of 8.5 per 100 skier seasons.2 Recreational skiers have the highest injury incidence.3 Other factors associated with ACL injury are high BMI, joint laxity, genetic predisposition, and muscle fatigue. Female skiers have a higher injury rate in comparison to male skiers. Environmental factors also have an impact on ACL injury risk. Skiing during icy conditions or during a heavy snowfall increase the risk of injury. This allows physicians staffing ski clinics to expect to see this injury based on the conditions they encounter traveling to work.5
Diagnosing
Most ACL injuries can be diagnosed through a careful history coupled with a good physical examination. Within the history, the skier often acknowledges hearing or feeling a "pop" with immediate pain. The pain often subsides quickly, and it is not uncommon for the skier to attempt to continue skiing only to realize that the knee feels unstable.
There are classic mechanisms of ACL injury. The most common in recreational skiers is the "boot-induced anterior drawer," where a quickly fired quad muscle pulls the tibia forward on the femur and tears the ACL, and the "phantom foot," where a skier falls backward and the inside ski catches the snow and twists the lower leg. More advanced skiers have other distinct ACL injury mechanisms, but most involve the skier leaning too far back.6
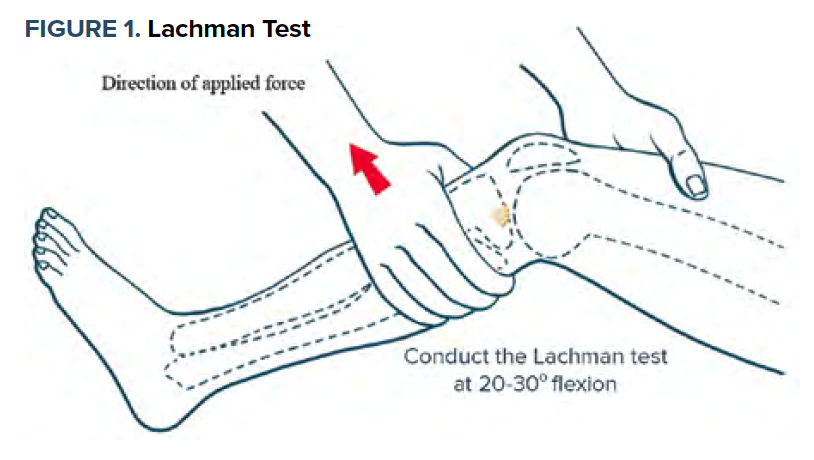
The best test for diagnosing an ACL injury is the Lachman test (sensitivity of 84% and specificity of 92%)7 (See Figure 1). Hold the knee in 20-30 degrees flexion. Stabilize the proximal femur with one hand and pull the proximal tibia anterior with the other, thereby inducing anterior translation of the tibia on the femur. A positive Lachman test is suggested by excessive anterior translation of the tibia with a "soft end point" in comparison to a "firm end point" when the ACL is intact.
There are other clinical tests available for assessing ACL injury:
- Anterior draw test (62% sensitive)
- Lever test (63% sensitive)
- Pivot shift test (most specific for ACL injury, but can cause severe pain on a fresh injury)9-11
While joint effusions and an antalgic gait are other classic findings, the bleeding from an ACL injury is slow, and an effusion usually is not present immediately after the injury. If you see a large effusion early, think about other injuries like tibial plateau fractures. Plain radiographs are used to rule out fracture. These fractures may be related to the ACL injury in the case of a Segond fracture (a small avulsion fracture of the anterolateral tibial plateau that is associated with ACL injury in approximately 75% of cases) or a tibial spine fracture.8 MRI can confirm the diagnosis and identify concurrent injuries.
Lachman: Getting It Right
The Lachman test sounds simple, but it can be tricky and takes practice to get correct. The key to performing a Lachman test is to get your patient to relax. Have them lay flat, relax their head back, and ensure their quads are loose. To achieve quadriceps relaxation you can place your knee or a pillow under the patient's knee as you do the exam. Finally, the Lachman test is much easier to do on someone with a small leg, so practice on your diminutive friends. You know you have it when you feel the ACL distinctively catch as you pull the tibia forward.
It is important to examine the unaffected knee; many patients have laxity that is not pathologic. It is also essential to evaluate the other knee structures that may be injured with the ACL. Many of you may recall the term "unhappy triad," which describes the simultaneous injury of the ACL, medial collateral ligament, and medial meniscus.
Injury Management
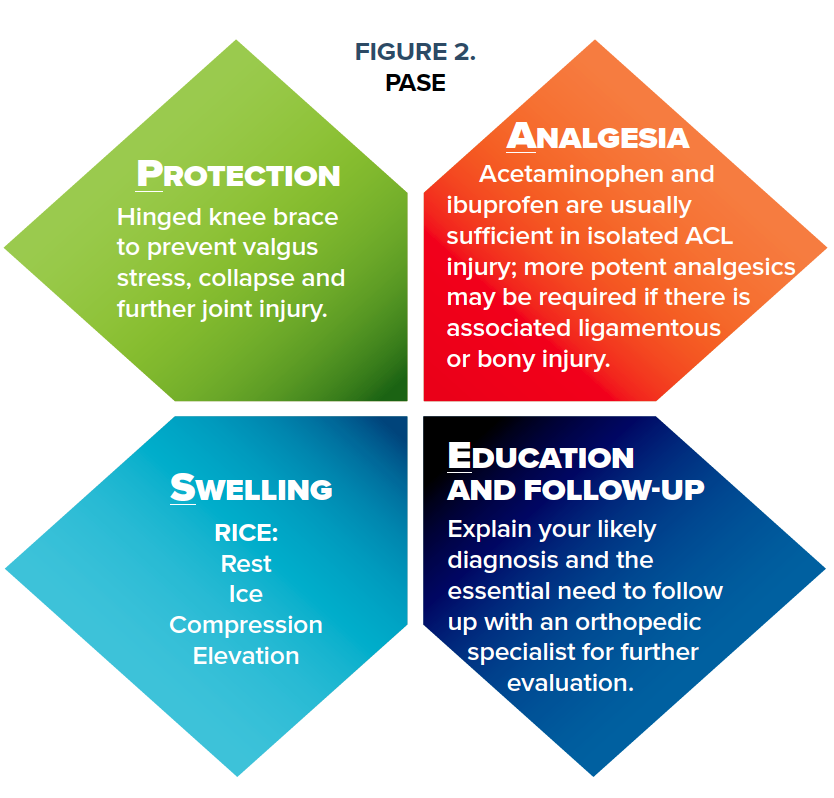
Management of ACL injuries is a hot topic in musculoskeletal medicine. There have been rapid advances in surgical approaches to ACL reconstruction and rehabilitation over the past decade. In a ski clinic, immediate priorities are simple: protection of the injured joint from further injury, analgesia, management of swelling/inflammation and good patient education: PASE (Figure 2).
If your patient is involved in activities that are primarily directed in a frontal plane, with little lateral movement, they can consider not having surgery. If they plan on doing activities with a high lateral stress load, they will usually do better with surgical reconstruction.
There is a tendency for people to develop quadricep inhibition and a decrease in knee range of motion (ROM) after an ACL injury. Before you discharge your patient, teach them to do focused quadriceps strengthening and ROM exercises. These exercises can be as simple as performing sets of heel slides, ankle pumps, straight leg raises, and knee extension exercises as they prepare for surgery.12
Finally, this injury can be an emotional hit for your patients. Recovery usually takes 6 months to a year. Plan a pep talk. Something like, "I know that an ACL injury sucks. We have great surgeons who are going to get your knee back together. You will be back skiing next year and I bet if you went into the lift line and asked everyone to raise their hand if they have had an ACL injury, 20-30% of them would have a hand up. You're gonna do great."
References
1. Stenroos A, Handolin L. Incidence of recreational alpine skiing and snowboarding injuries: Six years experience in the largest ski resort in Finland. Scand J Surg. 2015;104(2):127-31.
2. Pujol N, Blanchi MP, Chambat P. The incidence of anterior cruciate ligament injuries among competitive Alpine skiers: a 25-year investigation. Am J Sports Med. 2007;35(7):1070-1074.
3. Renstrom P, Ljunqvist A, Arendt A, et al. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;42(6): 394–412.
4. Smith H, Vacek P, Johnson R, et al. Risk Factors for Anterior Cruciate Ligament Injury. A Review of the Literature—Part 2: Hormonal, Genetic, Cognitive Function, Previous Injury, and Extrinsic Risk Factors. Sports Health. 2012;4(2):155–161.
5. Ruedl G, Ploner P, Linortner I, Schranz A, Fink C, Patterson C, et al. Interaction of potential intrinsic and extrinsic risk factors in ACL injured recreational female skiers. Int J Sports Med. 2011;32(8):618-22.
6. Bere T, Mok KM, Koga H, Krosshaug T, Nordsletten L, Bahr R. Kinematics of anterior cruciate ligament ruptures in World Cup alpine skiing: 2 case reports of the slip-catch mechanism. Am J Sports Med. 2013;41(5):1067-73.
7. Benjaminse A, Gokeler A, van der Schans CP. Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther. 2006; 36:267.
8. Goldman A, Pavlov H, Rubenstein D. The Segond fracture of the proximal tibia: a small avulsion that reflects major ligamentous damage. Am J Roentgenol. 1988;151(6):1163-1167.
9. Ostrowski JA. Accuracy of 3 Diagnostic Tests for Anterior Cruciate Ligament Tears. J Athl Train. 2006;41(1):120-121.
10. Jarbo KA, Hartigan DE, Scott KL, Patel KA, Chhabra A. Accuracy of the Lever Sign Test in the Diagnosis of Anterior Cruciate Ligament Injuries. Orthop J Sports Med. 2017;5(10).
11. Prins, M. The Lachman test is the most sensitive and the pivot shift the most specific test for the diagnosis of ACL rupture. Aust J Physiother. 2006;52(1):66.
12. Kim DK, Hwang JH, Park WH. Effects of 4 weeks preoperative exercise on knee extensor strength after anterior cruciate ligament reconstruction. J Phys Ther Sci. 2015;27(9):2693-2696.



