Case
You are working in Central America doing emergency development work, when a 7-year-old girl presents in status epilepticus. She has no seizure history or medical problems, though has been feeling ill for a few days with subjective fevers and headaches. She is febrile, unresponsive, without nuchal rigidity, equal and sluggish pupils, and has right-sided focal tonic-clonic movements. She is treated with benzodiazepines and is intubated. Her seizure activity slowly abates. The PICU attending is at the bedside and requests a lumbar puncture to rule out meningitis. You agree that a CSF sample would be ideal, however a focal seizure is very concerning for bleeding, mass, or brain abscess. If this patient has elevated intracranial pressure, a lumbar puncture may precipitate brain herniation. The PICU attending disagrees and says the hospital CT scanner is currently out of service anyway. If only there were another way to allay your concerns”¦
Discussion
The optic nerve is surrounded by cerebrospinal fluid (CSF) and dura mater forming the optic nerve sheath. The diameter of this sheath is measured as the optic nerve sheath diameter (ONSD) and is influenced by CSF pressure variations because it communicates with the subarachnoid space. Neuroimaging and direct invasive pressure measurement have long been used to measure intracranial pressure, with invasive intracranial devices being the gold standard for ICP measurement. Neuroimaging is not universally available and can lead to patient safety issues given time sensitive pathologic processes. Direct measurement has several disadvantages including its invasiveness, requirement of subspecialty training, infection, bleeding, and malfunction. As a rapid, non-invasive, readily available approach to evaluate elevated intracranial pressure, ultrasonography has been studied to reliably measure ONSD. A normal ONSD can rule out elevated intracranial pressure (ICP), though the exact cut off value for ONSD is not universally agreed upon.
The Evidence
Amini, et al. studied 50 non-trauma patients who were to receive lumbar puncture with opening pressures. They measured ONSD with ultrasound prior to the procedure. 14 patients were found to have elevated ICPs, and an ONSD diameter of >5.5 mm had 100% sensitivity and specificity for elevated ICP.1
Frumin, et al. used a prospective analysis with one emergency practitioner who ultrasounded 27 patients within 24 hours of placement of an external ventricular device. They found that an ONSD of >5.1 mm had a 83.3% sensitivity and 100% specificity for an ICP of >20 mmHg.2
Dubourg, et al. found the pooled sensitivity of ultrasound ONSD measurement for detection of increased ICP from six studies and 231 patients was 90%, with a pooled specificity of 85%. The pooled odds ratio was 51. The thresholds for defining elevated ICP by ONSD varied in these six studies from 5.0 mm to 5.9 mm. They all measured 3 mm from the posterior globe and all used high frequency transducers. The vast majority of patients found to have enlarged ONSD were diagnosed with traumatic brain injury, subarachnoid hemorrhage, or intracranial hemorrhage.3
Bauerle, et al. looked at patients with idiopathic intracranial hypertension (IIH), a different kind of population with chronically elevated ICPs. Ten subjects with recent diagnoses of IIH and 25 controls received both ultrasound measured ONSD and lumbar puncture. Using a cutoff value of 5.5 mm resulted in a 100% sensitivity for detecting raised ICP. Additionally, significant decreases in ONSD were observed after lumbar puncture.4 This study suggests ONSD responds well to real-time intracranial pressures, and that it may have a role for screening of IIH, and in the evaluation of headache.
Strumwasser, et al. studied patients with severe traumatic brain injury, and used invasive ICP monitoring to correlate with ultrasound measured ONSD. These subjects who required invasive ICP monitoring had ultrasound measured ONSDs ranging from 5.8 to 6.6 mm. This correlates well with elevated ICP based on current accepted thresholds. However, the study goal was not to screen for elevated ICP as an emergency physician might, but to evaluate for correlation of intracranial measurements before and after intervention. They found that ONSD poorly correlates with numerical intracranial pressure measurements. Therefore, ONSD cannot replace invasive intracranial monitoring.5
The Technique
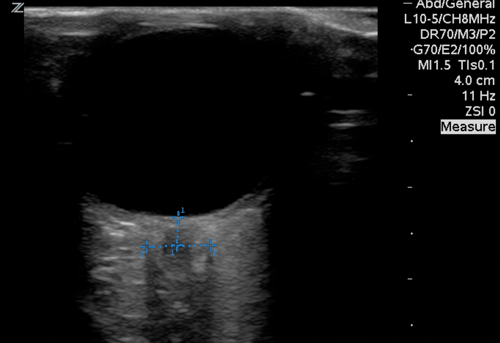
Using a high frequency probe and the “eye,” “ocular,” or “ophthalmologic” exam setting, place a transparent adhesive dressing bilaterally over the closed eyes. Place ample ultrasound gel in order to interrogate the eye in two planes. Rest a couple fingers on the patient's face for good control and be careful to not apply more than pressure than is required to the eye. Look for a hypoechoic structure extending from the optic disc into the posterior field. The nearly anechoic structure is the optic nerve, and the hypoechoic structure around it is the optic nerve sheath. Measure 3mm back from the optic disc and measure the diameter as demonstrated in Image 1. A reasonable ONSD value to rule out elevated ICP is 5.5 mm, although many clinicians are more conservative and use 5.0 mm. The traditional value of 5 mm is for those greater than 4 years old. Moretti, et al. noted from a review of the literature that values between 4 to 4.5 mm captured 83-100% sensitivity for elevated ICP in those less than 4 years old.6
Case Resolution
A bedside ultrasound is available. The patient's ONSD measures 7.2 mm on the left and 7.1 mm on the right. The LP is foregone, and the patient is stabilized and sent to another facility for CT imaging which shows a large left-sided brain mass with associated acute hemorrhages. The results are discussed with the family, and the patient is admitted to the PICU where she unfortunately decompensates and is made comfort care before expiring.
Conclusion
ONSDs have been correlated with elevated ICPs in multiple studies confirmed by invasive ICP monitoring, neuroimaging, and opening pressures on lumbar puncture. ONSD can evaluate patients for elevated intracranial pressure with excellent sensitivity, as demonstrated above. The technique is easy to perform and in the right clinical setting it can change clinical management. Furthermore, studies demonstrate that ultrasound can be used by expert practitioners to measure ONSD at the bedside with reasonable accuracy. Performance of ONSD measurement is well within the grasp of novice and seasoned emergency practitioners, and should be considered in the initial work-up of suspected increased ICP. Its ease of use, reliability, and non-invasiveness are significant advantages over the other methods of ICP acquisition. Along with fundoscopic exam, lumbar puncture, and advanced imaging, ONSD should make its way into the emergency medical provider's repertoire in evaluating a patient for elevated ICP. In the right clinical scenario, it might be the most appropriate modality available.
References
- Afshin Amini et al. Use of sonographic diameter of optic nerve sheath to estimate intracranial pressure. American J of Emergency Medicine 31, 236-239 (2013)
- Erica Frumin et al. Prospective Anaylsis of Single Operator Sonographic Optic Nerve Sheath Diameter Measurment for Diagnosis of Elevated Intracranial Pressure. Western J of EM, XV, no2, 217-220 (2014)
- Julie Dubourg et al. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: a systemic review and meta-analysis. Intensive Care Med 37:1059-1068, 2011
- Jochen Bauerle and Max Nedelmann. Sonographic assessment of optic nerve sheath in idiopathic intracranial hypertension. J Neurology 258:2014-2019 (2011)
- Aaron Strumwasser et al. Sonographic Optic Nerve Sheath Diameter as an Estimate of Intracranial Pressure in Adult Trauma. J Surgical Research, 170, 265-271 (2011)
- R. Moretti and B Pizzi. Ultrasonography of the optic nerve in neurocritically ill patients. Acta Anaesthesiology Scand 55: 644-652 (2011)