Paradoxical coronary emboli are rare phenomena that nevertheless should remain on your differential when patients with low risk factors for coronary artery disease develop atraumatic chest pain.
Case
A 25-year-old, thin West African male without any reported medical history presented for a chief complaint of chest pain. He was in his usual state of health when he developed an acute-onset crushing central chest pain that woke him up from sleep. He had associated shortness of breath with no prior history of similar symptoms. Pre-hospital care included 325 mg of aspirin and 2 sublingual nitroglycerin without changes in his symptoms. Pre-hospital EKG was concerning for possible inferior ST-elevation myocardial infarction (STEMI).
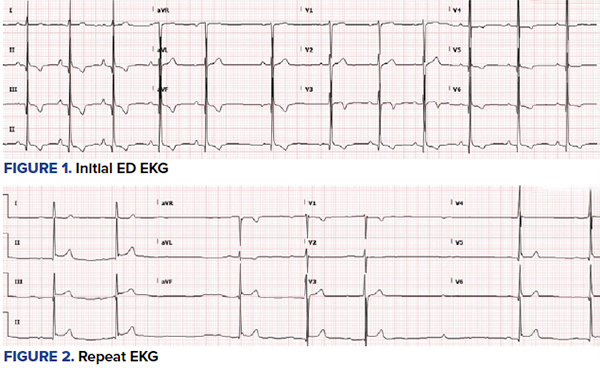
On initial presentation, the patient was in moderate distress, ill-appearing, and diaphoretic. Vital signs showed a heart rate of 58, blood pressure of 131/77, respiratory rate of 28-32, and saturating at 100% on room air. An EKG in the ED was obtained (Figure 1), which showed improvement of the initial ST-elevations in the inferior leads with inverted T waves in the inferior and anterolateral leads. While on telemetry monitoring, the patient went in and out of slow atrial fibrillation and high-degree heart block resulting in bradycardia in the 30s and associated lethargy. Interventional cardiology was consulted, but they did not recommend cath lab activation. Instead, they recommended further workup in the ED.
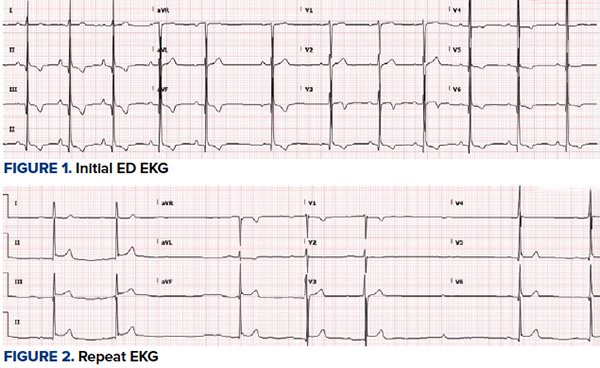
Bedside echocardiography was done showing subtle inferior wall hypokinesis with no significant right heart strain and no apparent aortic pathology. Interventional cardiology was called again, but they did not believe the patient warranted catheterization lab given his age and lack of cardiac risk factors. Repeat EKG was performed (Figure 2) which showed dynamic changes in ST-segments, T waves, and new arrhythmias. The patient continued to be symptomatic with chest pain and shortness of breath. Additional discussion with the interventional cardiologist was had regarding the patient’s continued presentation and findings. They continued to advise medical management and workup.
Additional history revealed the patient was a daily smoker with occasional marijuana use. The patient recently took a road trip to Texas 5 days prior. Although he was originally from West Africa, he had not had any recent foreign travel. There was no significant family history reported. All immunizations were up-to-date.


Given the initial limited history and presentation, a case for atraumatic chest pain in a young adult elicited a broad range of differentials. A comprehensive workup was obtained and the patient was started on a heparin drip. A CT head scan was unremarkable and CT chest scan was negative for pulmonary embolism (PE). The patient was admitted to the cardiac intensive care unit (CCU).
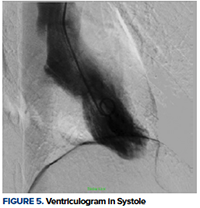
On CCU’s initial evaluation, he continued to be bradycardic with an intermittent high-degree heart block that was unresponsive to atropine therapy. The patient maintained good perfusion and mental status throughout this course. The second troponin at 3 hours increased from 0.07 to 1.38 and a CK-MB of 7. The decision was made to transport the patient to the cath lab for an angiogram. Results showed abrupt cut-off of the inferoapical segment of the left anterior descending artery (LAD), which was likely secondary to a clot embolism (Figures 3, 4). Preserved left ventricular systolic function with akinesis of the apical and inferoapical wall segments was noted on ventriculogram (Figure 5). The right coronary artery (RCA) was unremarkable. Given the extreme distal positioning of the embolism, no further interventional therapy was done at that time. Further workup with transthoracic echocardiogram complete with bubbles demonstrated Chiari network and a small patent foramen ovale (PFO). Extremity Dopplers showed no deep vein thrombosis. The patient’s blood test was negative for coagulopathies, viral or bacterial etiologies, and toxicology testing was negative for cocaine use.
Introduction
Patent foramen ovale (PFO) is traditionally recognized as a component of fetal circulation and closes shortly after birth. However, roughly 25-30% of individuals live with a PFO, with autopsies reporting prevalence at about 27%.5 A PFO potentially increases in size with each decade of life, subsequently increasing the risk of paradoxical embolism. Paradoxical coronary emboli are rare phenomena and account for approximately 5-10% of all paradoxical emboli.11 Various case reports have noted occurrences of paradoxical embolism in those who are at risk for thrombus formation including patients who are pregnant, have coagulopathies, history of cancer, or congenital heart disease, and even those who are mechanically ventilated.1,2,4,6,10 In the setting of a young healthy patient with no significant coronary artery disease, they are rarely reported and, thus far, there is no concrete epidemiology on the incidence or prevalence of acute myocardial infarction (AMI) caused by a paradoxical embolus.
Pathophysiology
Paradoxical embolism originates from the venous vasculature and transverses through an intracardiac (eg, PFO) or pulmonary shunt when right atrial pressure exceeds left atrial pressure (such as during Valsalva maneuvers) resulting in shunting of blood and passage into the systemic circulation.13
Paradoxical embolism in patients with PFO has been better studied and documented in cases of cerebrovascular accidents and peripheral vascular occlusions with fewer data looking at AMI. Prior literature evaluating the incidence of PFO in patients with AMI and angiographically normal coronary arteries demonstrated no significant increase in prevalence of PFO, suggesting that paradoxical embolism through a PFO is a rare cause of AMI.3 Similarly, to date, it has not been shown that having a right-to-left shunt is an independent risk factor for AMI.7 This is likely due to the low frequency of these events along with the underreported amount of cases, which make it difficult to establish any controlled studies of significant power.
Additionally, there is always the possibility that the presence of a PFO was found incidentally without a true cause-effect relationship with the AMI. This is a frequently debated topic as a visualization of a thrombus within the PFO is not always feasible. However, we do know this is a plausible physiologic mechanism. Prior literature has evaluated PFO as a potential pathway into additional vasculatures, such as the coronary arteries, which included the histopathological evaluation of the thrombus.8,9,13
Case Discussion
This case presented with multiple pathophysiologic points that did not follow the typical statistical and physiological variant for ACS. The patient had a seemingly unprovoked embolus that formed and traveled through a small PFO into the left heart during a momentary right-to-left shunting process. The embolus subsequently was not pushed out into the systemic circulation during systole and instead went into the left coronary artery during diastole when the ventricle relaxed and allowed for filling of the coronary arteries. Furthermore, the initial primary concern was for RCA involvement. This patient had dynamic EKG changes along the inferior leads, bedside echocardiogram was notable for inferior wall motion abnormality, and intermittent episodes of high degree heart block on telemetry monitoring. Approximately 90% of the population’s AV node is supplied by the RCA. This patient, however, had a LAD that supplied down to the inferoapical wall, which reproduced similar findings of RCA involvement.
Currently, there is a dearth of literature to guide initial management of a paradoxical coronary artery embolism causing AMI. Standard treatment and prevention also remain unclear with guidelines that do not take non-cerebral embolic events into account. Nevertheless, options to be considered are percutaneous angioplasty/stent placement, thrombolysis, or thrombus aspiration embolectomy.
Case Conclusion
The patient continued to remain stable and was further monitored with anticipation of PFO closure. Paradoxical coronary artery embolism through a PFO causing AMI is rare and often underdiagnosed. A high degree of clinical suspicion should be had in patients with atraumatic chest pain who have low or no risk factors for coronary artery disease.
References
- Agostoni P, Gasparini G, Destro G. Acute myocardial infarction probably caused by paradoxical embolus in a pregnant woman. Heart. 2004;90(3).
- Croft AP, Khan JN, Chittari MV, Varma C. Paradoxical coronary artery embolism causing acute myocardial infarction in a young woman with factor V Leiden thrombophillia. J R Coll Physicians Edinb. 2012;42(3):218-220.
- Crump R, Shandling AH, Van Natta B, Ellestad M. Prevalence of patent foramen ovale in patients with acute myocardial infarction and angiographically normal coronary arteries. Am J Cardiol. 2000;85(11):1368-1370.
- Hakim FA, Kransdorf EP, Abudiab MM, Sweeney JP. Paradoxical coronary artery embolism - A rare cause of myocardial infarction. Heart Views. 2014;15(4):124-126.
- Hara H, Virmani R, Ladich E, et al. Patent foramen ovale: current pathology, pathophysiology, and clinical status. J Am Coll Cardiol. 2005;46(9):1768-1776.
- Jamiel A, Alsaileek A, Ayoub K, Omran A. Paradoxical embolism in acute myocardial infarction in a patient with congenital heart disease. Heart Views. 2012;13(3):111-113.