Ch. 15 The Sick and Undifferentiated Medical Patient
At 17:00, two paramedics respond to the home of a 65-year-old man for a ‘sick’ call type. No other dispatch information is available for the crew pre-arrival. On scene, the patient states he feels “unwell” but is unable to better characterize his symptoms other than mild nausea. He has a PMH of chronic back pain and no other medical problems, with infrequent primary care visits. He denies any specific complaints other than his typical back pain. His wife reports that he was acting normal earlier today and she doesn’t know what’s wrong with him. She’s a bit surprised he asked her to call 911, saying “He wasn’t really complaining all that much.” He takes naproxen for his back pain, which generally alleviates the pain. He denies any allergies or prior surgical history.
EMS providers rely on the initial dispatch information to guide their assessment and treatment on scene such that faulty dis- patch information may steer EMS providers down the wrong path, wasting valuable time and leading to ineffective or inap- propriate prehospital care. Thus the role of CRO is critical as the initial part of the EMS chain to provide the prehospital standard of care.
Emergency Medical Dispatch (EMD)
A medical call-receiving operator (CRO) trained in EMD has limited time to accurately identify the chief complaint and obtain vital medical information from the 911 caller. They are trained to collect information in a structured manner to perform priority dispatch. Due to callers’ heightened anxiety or altered mental status, unreliable or misleading information is often transmitted to the responding EMS crews.
Undertriaged dispatch: Inappropriate or unprepared resources rendering substandard level of care (eg, BLS providers respond- ing to a “sick” call type that turns out to be a patient in severe respiratory distress.
Overtriaged dispatch: Excessive resources responding with lights and sirens, which puts the public and responders at risk and at great cost to the 911 system, to a stable patient (eg, first responders, BLS ambulance, ALS ambulance, EMS supervisor re- sponding to a “Cardiac Arrest” call that turns out to be a person sleeping).
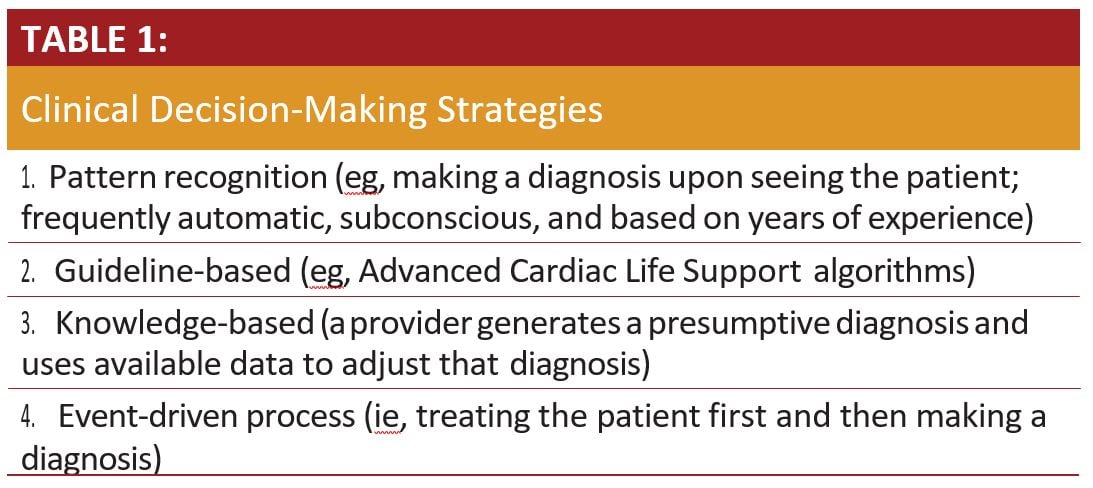
Clinical Decisions
EMS providers must accumulate a great deal of information in a short time period. They then incorporate this information with their clinical skills and exam into their clinical decision-making. Delays in treatment and transport can impact patients’ morbidity and mortality. Providers must make quick decisions based on limited information while providing thorough and efficient care. This has been termed heuristics. There are 4 main strategies that providers use in clinical decision-making (Table 1).
History and Physical
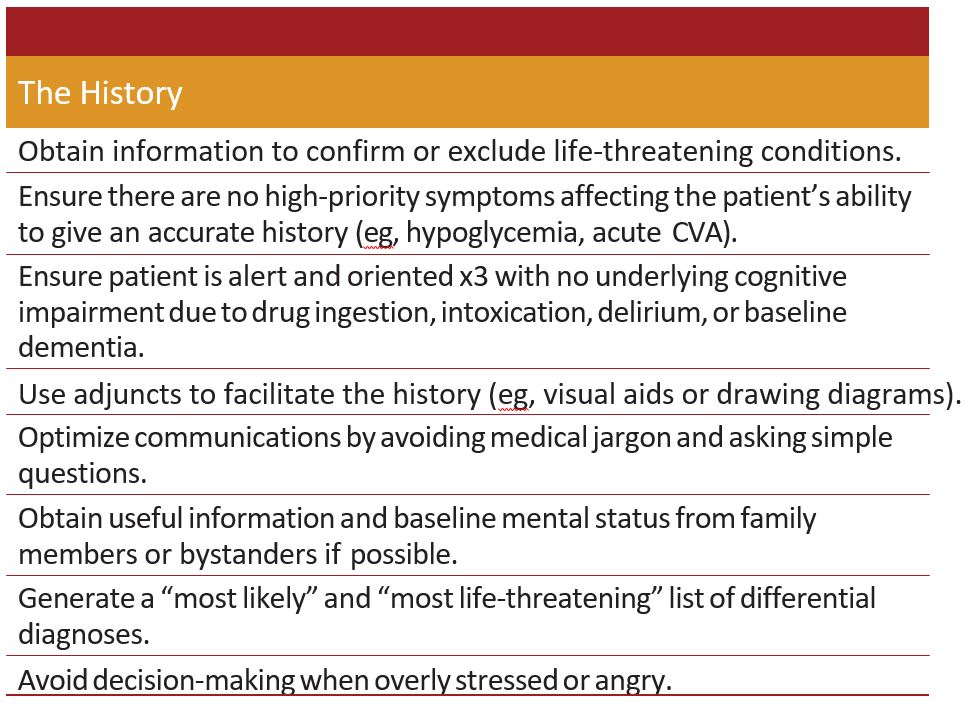
Field personnel must acquire a detailed and unbiased history using effective communication strategies. Regardless of the dis- patch information, providers should approach each patient in the same manner. A balance of open-ended (Can you describe your pain?) and close-ended (Is your pain sharp or dull?) questions will produce a sufficient, succinct history. Traditional teaching pro- fesses that a diagnosis can usually be made by a thorough history alone.
When assessing a patient with an undifferentiated dispatch code, EMS providers identify a prehospital chief complaint and treat the patient in accordance with the regionalized protocols. Occasionally, however, providers are unable to identify a specific prehospital chief complaint leading to the “undifferentiated” prehospital patient. If the patient is undifferentiated after ob- taining a detailed history, providers follow the strategies listed in Table 2.
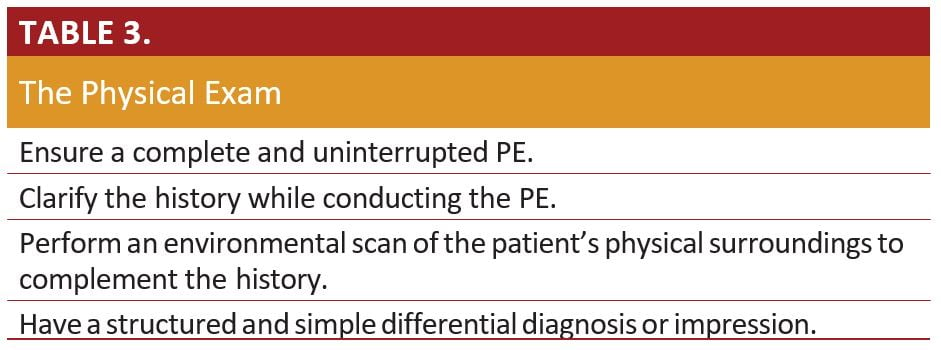
If patients remain undifferentiated despite a thorough histo- ry, providers should perform a thorough physical exam (PE) to augment the history that has been elicited. Obtaining a complete set of vital signs is the first step of a physical exam. Afterwards, utilize the strategies listed in Table 3.
Diagnostic Assessment
If the history and physical exam have not collectively iden- tified a chief complaint, providers should use appropriate pre- hospital diagnostic tests to facilitate a working diagnosis, such as a point of care blood glucose level or 12-lead ECG. Some EMS systems offer prehospital point of care lactate testing to assist the providers in their differential diagnosis (eg, early diagnosis of sepsis). When crews have identified an undifferentiated patient, they should minimize the time to transport while continuing to obtain information and reassessing vital signs as warranted.
Knowing the importance of a good transition of care to the triage nurse, especially with an undifferentiated patient, the crew clearly explains they do not have a presumptive diagnosis. Importantly, they note, he just had one episode of emesis prior to arrival and an acute worsening of his chronic back pain. The senior paramedic states, ”I’m not sure what’s going on with him, and that makes me even more con- cerned about him.” The triage nurse listens to their assessment and obtains a new set of vital signs: 105/70, 110, 20, 97%. The EMS providers astutely notice the drop in blood pressure since their previous mea- surement, which prompts the nurse to triage the patient into the critical care area of the ED. After evaluation by the ED staff, and with the benefit of a bedside ultrasound, a ruptured abdominal aortic aneurysm is quickly diagnosed. As the crew walks out of the ER, they realize the quality care they provided led to a quick diagnosis of a critical condition and any delay in assessment, treatment, or transport would have resulted in missing this critical life-threatening event.